What is Noonan syndrome?
Noonan syndrome is a genetic condition that occurs in about 1 in every 1000–2500 children. It is equally present in both males and females and in all parts of the world.
Signs and symptoms of Noonan syndrome
Noonan syndrome can affect different parts of the body. Individuals with Noonan syndrome may have only a few or many of the physical or developmental differences listed below:
Face and neck
-

Top: Widely-spaced eyes. Bottom: Eyes with ptosis (droopy eyelid). Widely-spaced eyes or abnormalities of the eyes and eyelids that may or may not affect vision (e.g., ptosis)
-

Flattened nasal bridge
-

Oval-shaped, low-set ears
-

Increased nuchal fold (area at the nape or back of the neck)
-

Top: A normal neck. Bottom: Broad neck with excess skin. Broad neck with excess skin (webbed neck)
Skeleton and limbs
-

The orange dotted line represents the curve in the child's spine (scoliosis). The solid orange line shows where the child's spine should be straight. Abnormal side-to-side curvature of the spine (scoliosis).
-

On the left is an example of a sunken chest. On the right is an example of a protruding chest. Sunken chest (pectus excavatum) or a protruding chest (pectus carinatum)
- Short stature
- Swollen hands and feet (lymphedema) usually seen in infants
Brain
- A spectrum of learning difficulties
- Impaired hearing
- Delayed milestones
Genitals
- Undescended testicles
- Delayed puberty onset
Feeding and nutrition
- Feeding difficulties in infants and small children
Blood
- Increased tendency to bleed
- A rare but increased risk of some types of cancer
Causes of Noonan syndrome
Noonan syndrome is caused by one of several genes that play a key role in the normal functioning of cells. At least 12 genes have currently been associated with Noonan syndrome.
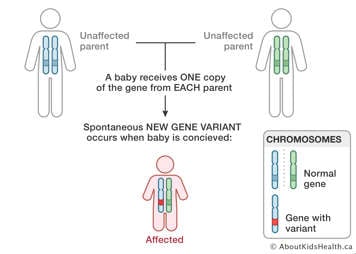
In most cases (60%), Noonan syndrome is caused by a genetic change (variant) that occurs for the first time (de novo) in the child.
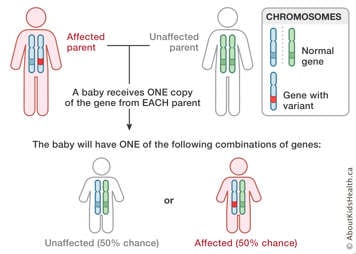
Noonan syndrome can also be inherited from a parent. Most cases of inherited Noonan syndrome are inherited in an autosomal dominant manner. This means that if a parent has Noonan syndrome, there is a 50% chance in each pregnancy to have a child with Noonan syndrome.
When the genetic change occurs de novo in the child, there is a less than 1% chance for the parents to have another child with Noonan syndrome.
There are a number of options for genetic testing either prior to or during a pregnancy for families that have an increased chance to have a child with Noonan syndrome. A genetic counsellor can help review these options.
Diagnosis of Noonan syndrome
The diagnosis of Noonan syndrome can be made either clinically or by genetic testing. A genetic change associated with Noonan is found in about 80-85% of individuals with Noonan syndrome. This means that a negative genetic test does not rule out the diagnosis. Genetic testing has important implications for genetic counselling and management.
Treatment of Noonan syndrome
There is currently no single treatment for Noonan syndrome, but it is often possible to successfully manage several aspects of the condition. Studies are underway for novel treatments.
Every child with Noonan syndrome is different and many go on to lead normal lives. Some children with Noonan syndrome can have delayed milestones or learning difficulties. However, when recognized early, they respond well to additional support. Children with Noonan syndrome typically also require regular follow-up by several medical specialties.
Patients with heart conditions may require a heart intervention or surgery, depending on the symptoms and severity of the condition. The treatment will depend on the specific heart defect. With pulmonary stenosis, the aim is to relieve the thickening of the valve and to make it easier for the blood to flow from the heart to the lungs. This can be achieved by a cardiac catheter (e.g. balloon dilation) or, more frequently, by cardiac surgery (open-heart surgery). For information on treatment of hypertrophic cardiomyopathy, please see the article Hypertrophic cardiomyopathy.
Heart conditions associated with Noonan syndrome
About 80% of Noonan syndrome cases involve a heart condition. These conditions fall into two main categories: congenital heart disease (about 80% of cases involving a heart condition) and hypertrophic cardiomyopathy (about 20% of cases involving a heart condition).
Congenital heart disease: Pulmonary stenosis
Pulmonary valve stenosis is the most common heart condition associated with Noonan syndrome, seen in up to 70% of cases. The pulmonary valve controls the blood flow from the heart to the pulmonary artery, which then leads to the lungs so the blood can get oxygen. Stenosis means that the valve is thick and its opening is narrower than normal, which makes it hard for the blood to flow through it.
In most cases this pulmonary valve narrowing is only mild and will not cause your child to have any symptoms or to require any intervention. Your child’s doctor might hear a murmur as they listen to your child’s chest. This is related to the turbulence of the blood as it crosses the thickened valve.
Less frequently, the pulmonary valve narrowing may be moderate or severe. These cases might require a cardiac intervention or a surgery.
Congenital heart disease: Other heart defects
Other heart defects may occur in Noonan syndrome patients, although this is less common. The majority of these defects are related to the abnormal formation of the walls that divide the left and the right sides of the heart. The atria are located in the upper part of the heart. The wall that separates the right and left atria is called the atrial septum. A defect (hole) in this wall is called an atrial septal defect (ASD). The majority of ASDs will produce no symptoms at first and might only be detected due to a murmur.
The ventricles (the pumping chambers) are located in the lower part of the heart. The wall that separates the right and left ventricles is called the ventricular septum. A defect in this wall is called a ventricular septal defect (VSD). Depending on the size of this hole, your child might have no symptoms at all or present with heart failure symptoms. This lesion will also produce a murmur that your child’s doctor may be able to hear with a stethoscope (auscultation). For more information on heart failure please see aboutkidshealth.ca/heartfailure.Hypertrophic cardiomyopathy
Hypertrophic cardiomyopathy is a condition in which the heart muscle becomes unusually thick. This can affect the amount of blood pumped to the body and cause heart rhythm problems. Many patients with this condition may not experience any symptoms at all, the only sign being a heart murmur on auscultation. Some patients may have shortness of breath, chest pain, dizziness, fainting, palpitations and, in rare cases, cardiac arrest. For more information please see the article Hypertrophic Cardiomyopathy.