What is anemia?
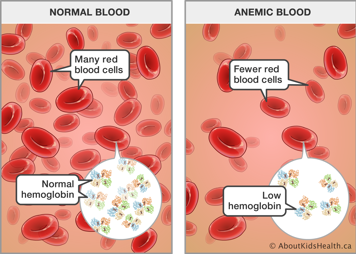
Anemia is a lack of either hemoglobin or red blood cells in the body. Hemoglobin is the iron-rich protein in red blood cells (RBCs) that allows transport of oxygen to all the cells in your body. Every cell in the body needs oxygen.
Anemia occurs when the amount of hemoglobin in a person's blood is too low. This means there is not enough delivery of oxygen to the body.
Anemia can last a short time or a long time. Treatment depends on the cause of the anemia.
Signs and symptoms of anemia
Symptoms depend upon the severity of the anemia, how fast the drop occurred, and its cause. It also depends on how well a child's body adapts to a low level of hemoglobin. Symptoms may include:
- pale skin, because hemoglobin causes blood to be red coloured
- lack of energy, because of reduced oxygen in the body
- shortness of breath after exercise or play, due to lack of oxygen in the body
- fast heart rate, since the heart needs to work harder to deliver oxygen to the rest of the body
Causes and types of anemia
There are several types of anemia. In general, they are classified by cause.
Nutritional anemias
Iron deficiency anemia is the most common type of anemia. It is caused by a lack of iron in the diet. Iron is needed to make hemoglobin. Term infants fed only breast milk, non-iron fortified cow milk formulas or whole cow's milk may be at risk for iron deficiency after six months of age. Breast milk or iron-fortified formula is a good source of iron for the first six months of life. Iron stores in babies naturally decrease by four to six months of age. The iron in breast milk is well-absorbed, but after six months, the amount of iron in breast milk is not enough, and solid foods that contain iron are usually introduced. Premature infants often develop anemia earlier due to reduced iron stores at birth.
Iron deficiency anemia can also occur in children due to chronic blood loss from the gastrointestinal tract, such as in inflammatory bowel disease (ulcerative colitis and Crohn’s disease) or cow’s milk protein allergy. It can also occur due to difficulty absorbing iron in the small intestine, such as in celiac disease.
Less commonly, vitamin deficiency can cause anemia. Vitamin deficiency anemia is a lack of folic acid, vitamin B12 or vitamin E in the diet. The body needs all these nutrients to make hemoglobin.
Anemias caused by disease
Anemia due to abnormal hemoglobin (hemoglobinopathies)
Sickle cell disease is an inherited condition that causes RBCs to be an abnormal shape. These cells cannot flow through the body as well as normal RBCs. These RBCs don’t live as long as regularly shaped RBCs. This can lead to less delivery of oxygen to the body.
Thalassemia is another inherited hemoglobinopathy that leads to small RBCs that do not live long, leading to anemia. There are various forms of thalassemia, and the severity of anemia differs among them.
Hemolytic anemia
Hemolytic anemia describes a group of conditions that lead to destruction of the RBCs. Hemolytic anemia may be inherited, such as in G6PD deficiency or hereditary spherocytosis, or it may be acquired, such as in autoimmune hemolytic anemia (AIHA). Autoimmune hemolytic anemia can occur when a child’s immune system is activated to destroy RBCs. This may happen on its own for no clear reason and can also occur after certain infections or medications.
Anemia of chronic disease
Anemia of chronic disease can be found in children with many chronic conditions, such as chronic kidney disease, cancer, lupus and systemic juvenile idiopathic arthritis.
Aplastic anemia
Aplastic anemia is a rare and serious disease causing the body to stop making enough new blood cells. A child may be born with this type of anemia or may develop it after a viral infection or exposure to certain medications.
Risk factors for anemia
There are some groups of children that have a higher risk of developing anemia. Factors that may cause a higher risk include:
- family history of inherited anemia
- prematurity and low birth weight
- recent immigration from the developing world
- excessive consumption of cow's milk
- bottle feeding beyond 18 months of age (this often leads to excessive consumption of cow’s milk)
- vegan and vegetarian diets
- food insecurity
- chronic illness
What your child's health-care providrer can do about anemia
Your child's health-care provider will examine your child and ask you about their energy level, general health and family history. A detailed nutrition history is also very important.
A blood test called a complete blood count (CBC) will show the amount of hemoglobin in your child's blood to see if your child has anemia. Other blood tests may be needed to confirm the specific type of anemia.
Treatment of anemia
Treatment depends on how severe your child's anemia is and what is causing it. Common treatments include:
- iron supplements
- infant iron-rich formula
- dietary changes, such as reducing milk and increasing iron
- Iron rich foods include meat and green vegetables. A child who does not eat meat should eat plenty of green vegetables such as kale, spinach, collard greens and artichokes.
- folic acid and vitamin B12 supplements
Anemia caused by a more serious disease may require:
- intravenous iron infusions
- blood transfusions for certain types of anemia
- treatment to make the bone marrow produce more blood cells
- treatments for specific chronic diseases
Long term effects of anemia
Untreated anemia in children can have a serious effect on a child's growth. Anemia may affect brain development and function. This often leads to attention problems, delays in reading ability, poor school performance and in very rare cases - stroke.
When to seek medical assistance
Call your child's health-care provider if:
- your child appears pale and tired
- you suspect your child may have anemia