What is irritable bowel syndrome?
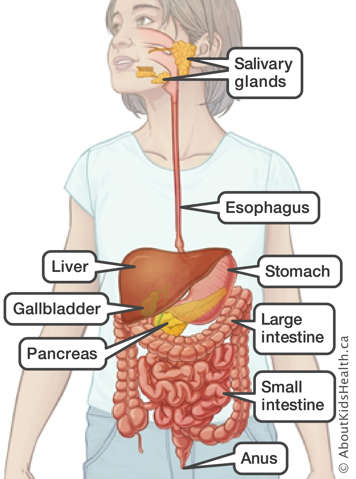
Irritable bowel syndrome (IBS) is a chronic condition of the large intestine (colon). The cause of IBS is unknown. It is probably not a single disease, but a combination of factors that cause a collection of symptoms. IBS is considered a so-called ‘disorder of gut-brain interaction’ (DGBI) meaning the digestive system looks normal but is not working as it should. It is likely sending and receiving jumbled nervous system messages to and from the brain, or the brain is interpreting those signals incorrectly. In IBS, food moves through the colon too slowly, quickly or unpredictably. As a result, water absorption by the colon is disrupted causing abdominal pain along with diarrhea or constipation.
Symptoms of IBS vary
Symptoms can flare-up, disappear and change over time. Common symptoms include:
- stomach pain or discomfort (cramping)
- bloating
- a changed need to go to the bathroom: either more often or less often
- change in consistency of stools (diarrhea, constipation)
- symptom relief after bowel movements
IBS is not known to lead to other serious health problems. However, IBS can affect mental and social well-being if not well managed.
Common IBS triggers
The cause of IBS is also unknown but viral gastroenteritis, stress, some foods and medications can trigger symptoms.
Foods that trigger symptoms may include:
- foods high in insoluble fibre (raw fruits and vegetables, whole grains, bran, legumes)
- dairy products
- nuts, seeds and raisins
- chocolate
- spicy food
- coffee or other caffeinated beverages
- carbonated beverages
- alcohol
- artificial sweeteners (aspartame, sorbitol, sucralose, xylitol, maltitol)
Other factors may increase IBS symptoms by over-stimulating the bowels. These may include:
- high-fat or very low-fat diet
- eating large meals
Diagnosing IBS
Diagnosing IBS may not be simple because the colon often looks normal. Often, tests eliminate the possibility of other intestinal disease. IBS may run in families.
In order to diagnose IBS, a child’s abdominal pain must occur for at least four days per month for at least two months along with one or more of the following criteria:
- pain is related to a bowel movement (poop)
- there is a change in stool (poop) frequency or appearance (such as looser or firmer)
- in children with constipation, abdominal pain does not improve or resolve after constipation is treated
- symptoms cannot be explained by another medical condition
IBS and IBD are not the same thing
IBD and IBS are very different, even though some symptoms overlap. IBD stands for inflammatory bowel disease. Although some symptoms between IBS and IBD are the same, IBD has other significant symptoms that make it different from IBS. IBD is often diagnosed with much more confidence and has specific treatments. It is common to misdiagnose IBD as IBS without a thorough examination.
Children with IBS have no inflammation of their gastrointestinal tract. IBS is not associated with poor growth or weight loss.
Managing IBS
There is no cure for IBS, but symptoms can be managed. How IBS symptoms are best managed varies from person to person. Your child may have to try different things to discover what works for them.
Keep a detailed diary
One thing you can do is to keep track of:
- what your child eats and when they eat it
- the frequency and consistency of stools
- events and activities
- timing and description of symptoms
If you have a detailed daily diary like this, it will help not only with diagnosis but also with making changes in your child's life to reduce the impact of symptoms. Routine restriction of certain types of food is not recommended in IBS. However, specific elimination of highly suspicious triggers can be considered under the supervision of a dietitian to ensure nutritional requirements are still being met.
Lifestyle changes
Encourage your child to:
- get enough sleep and exercise
- avoid stress as much as possible
- avoid eating on-the-run or skipping meals
Dietary changes
Encourage your child to:
- eat small and frequent meals during the day
- avoid large meals
- eat meals slowly
- eat higher protein and lower fat meals
- limit eating processed or greasy foods
- eat foods with plenty of soluble fibre (oat bran, corn, legumes, beans, oranges, apples, pears, berries, ground flax seeds)
- drink water regularly
Low FODMAP diet
FODMAPs are types of carbohydrates that are poorly absorbed in the intestines and may lead to gas production, bloating and distention. Foods that are high in FODMAPs, such as specific fruits, vegetables and grains, may lead to more symptoms, while foods that are lower in FODMAPs may help reduce symptoms triggered by food. The role of a low FODMAP diet in IBS has been studied in adults. While many adults with IBS try a low FODMAP diet, it is not recommended for all children with IBS because fewer studies have been done in children. There is a higher risk that severely restricting groups of foods in children may affect their growth. In certain instances, some children with IBS may be advised to try a low FODMAP diet under the supervision of a dietitian.
A note on insoluble fibre
Insoluble fibre is important for regular bowel movements, but it may cause symptoms for people with IBS. Introduce it in small amounts to find out how much your child can eat and stay symptom-free. Try to peel, cook, chop or puree fruits and vegetables. This will reduce the effect of insoluble fibre on your child’s intestines. Sources of insoluble fibre include whole grains, brown rice, rye, whole flax seeds, vegetables, fruit and corn.
Some other common treatments of IBS
- Probiotics (taken as a pill or powder).
- Cognitive behavioural therapy (by a mental health care provider) to improve the interpretation of signals sent between the brain and gut, and to reduce the risk of stress triggering gut symptoms.
- Specific types of antidepressant medications that also act to change the nervous system signals between gut and brain.
- Medications or natural foods that can reduce pain and bowel spasms.
When to seek medical attention
Speak to your child’s health-care provider if your child:
- has repeated episodes of abdominal pain with either diarrhea or constipation several times a month for at least two months
- if your child has daily loose, frequent watery stool for more than two weeks
- your child has weight loss or bloody diarrhea