What is a patent ductus arteriosus?
In the womb, baby's oxygen comes from the mother. Since there is no need for blood to pass through the lungs of the fetus, the blood is diverted away from the lungs, to the rest of the body, by an artery called the ductus arteriosus.
Once a baby is born and takes their first breath, the ductus arteriosus is no longer needed and begins to close. Under normal circumstances, the ductus arteriosus is completely closed in a few weeks.
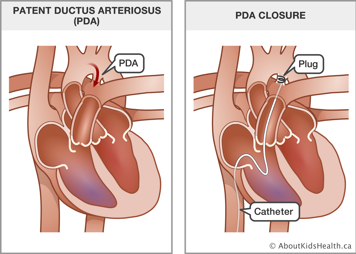
With some babies, this process of closure either does not happen at all or does not happen completely, leaving a small opening. As a result, normal blood flow is affected. This condition is called patent ductus arteriosus (PDA). Patent, in this context, means open.
Sometimes, the body just needs a little extra time for the PDA to close. Certain medications can also be used to encourage a PDA to close. If time or medications do not close the PDA, heart catheterization or surgery may be used. This information describes what happens during heart catheterization to close a PDA.
What is heart catheterization?
During heart catheterization, the doctor carefully puts a long, thin tube called a catheter into a vein or artery in your child's neck or groin. The groin is the area at the top of the leg. Then, the catheter is threaded through the vein or artery to your child's heart.
The doctor who does the procedure is a cardiologist, which means a doctor who works on the heart and blood vessels. This may not be your child's regular cardiologist.
There are small risks of complications from the procedure
Generally, heart catheterization is a fairly low-risk procedure, but it is not risk-free. The doctor will explain the risks of heart catheterization to you in more detail before you give your consent for the procedure. The most common risks with PDA closure are as follows:
The catheter may break through a blood vessel
There is a very small risk that the catheter may break through a blood vessel or the heart wall. To reduce this risk, we use a type of X-ray called fluoroscopy to see where the catheter is at all times.
Complications may occur with the closure device
While the device is being put in position, there is a risk that it may be put in the wrong place, move or fall out of the PDA. If this happens, the cardiologist will try to put it back in place. If this is not possible, surgery will be arranged to take out the device and close the PDA.
A more common complication is a small leak through the closure device. Usually this disappears with time. In rare cases, a second device may be placed over the first to stop the leak completely.
What does the closure device look like and how does it stay in place?
The closure device is made of metal and mesh material. It looks like a short tube with different-sized discs (circles) on either end. Before it is put in, the discs are folded so the device will fit in the catheter. When it is in the right place, one disc opens up as the device is moved out of the catheter. The tube portion plugs the PDA, and the other disc opens up on the opposite side. The PDA is now closed, with the device acting as a plug. This stops the blood from flowing through the PDA.
What happens during the procedure
The procedure is performed while your child is under a general anaesthetic. This means that your child will be asleep during the procedure.
During the procedure, the doctor inserts a catheter into a blood vessel in the groin at the top of your child's leg. The catheter is moved up the blood vessel into the heart and into the PDA. An X-ray picture is then taken of the PDA. A closure device is threaded through the catheter and placed into the PDA.
Once the device is in place, the doctor takes out the catheter and covers the cut on your child's leg with a bandage.
The procedure takes about one to three hours
The procedure usually takes one to three hours. After the procedure, your child will go to the recovery room for one to six hours to wake up from the anaesthesia.
After the procedure
The cardiologist will let you know when your child can go home. Your child will stay in the hospital for at least four to six hours after the procedure. Most children can go home on the same day as the procedure.
If your child needs to stay overnight, they will be transferred to the inpatient unit.
Your child will need to have an X-ray the morning after the procedure to make sure the closure device has not moved. If your child goes home overnight, you will need to bring your child back in the morning to have the X-ray.
Coming back for a check-up
Your child will be given an appointment to see the cardiologist six months after the procedure. At this time an echocardiogram, which is a type of ultrasound of the heart, will be done to ensure that the PDA is properly closed.
Write the date and time of the appointment here:
Antibiotics to prevent infectious endocarditis
Your child will need antibiotics before and after dental treatments for six months after the procedure. These drugs help prevent a heart infection called infectious endocarditis. Your child's cardiologist will tell you if this is needed for a longer time.