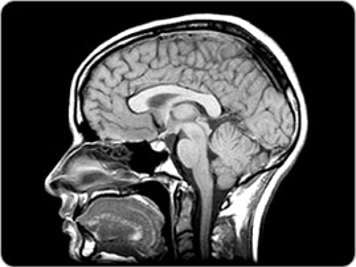
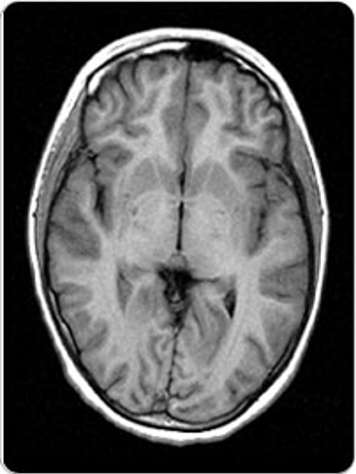
Magnetic resonance imaging (MRI) is a type of diagnostic imaging. The MRI machine scans the brain in “slices” to produce images. Each image shows a different “slice” or level of the brain. They are also called cross-sectional images. These images or scans are interpreted by a specialized doctor called a radiologist. An MRI machine does not use radiation or X-rays. A magnet, radio signals, and a computer are used to create the pictures. An MRI scan is fairly noisy but does not hurt. A number of short scans make up a complete MRI study. Each scan takes from one to 10 minutes. The total time for a complete MRI study is about one to two hours. An MRI can be done on any area of the body.
Is there any preparation for MRI?
If your child is old enough and able to lie perfectly still for an hour, then no special preparation is usually needed for the scans. However, many children need medicine to help them sleep so they will lie still for the scan. Also, if your child is afraid of enclosed spaces, let your treatment team know as they may require sedation. The type of sedation your child needs depends on your child's age and medical condition. Some children have a sedative by mouth and others will receive a general anaesthetic.
Before having any sedation or general anaesthetic, your child will have to be careful about what he eats or drinks. He will need to stop eating and drinking sometime before the sedation is given. The treatment team will tell you when your child needs to stop eating and drinking before the MRI.
Your child may have to wear hospital clothing or a gown during the scan.
Who will be doing the MRI study?
A team of three or four people will be doing the MRI study. A medical technologist trained in MRI will do the MRI scans. A nurse will prepare your child for the scans. She will give your child the sedation or help the anaesthetist. The anaesthetist is the doctor who gives the general anaesthetic. A radiologist will be checking and interpreting each scan to make sure that the study is complete. A radiologist is a doctor who specializes in interpreting diagnostic images.
Will my child be given any needles for the MRI study?
Most children having MRI scans will be given a needle. Children who are being sedated or are having a general anaesthetic will in most cases need to get a needle. Some MRI scans give the doctor more information when they are done with a special liquid called a contrast fluid. This clear, colourless fluid is given to your child through a small tube or needle inserted into a vein in the hand or arm (intravenous or IV). The liquid is quite safe. If the radiologist feels that your child’s scan would be better with this liquid, it will be given partway through the study.
What should I tell my child?
Tell your child exactly what will happen when the MRI scan is being done. This is explained in the section below. Explain what they will see, hear, and feel. Remember, MRI scans do not hurt but they are noisy.
What happens during the MRI?
Before you enter the room, you will be questioned or you may have to fill out a screening form. Staff need to make sure that it is safe for you to be near the strong magnet in the MRI scanner. You will have to empty your pockets completely of everything, including coins, keys, pens, wallets, and bank cards. You will also have to take off your watch.
Generally, parents may stay in the room during the MRI scan, but parents may not go into the room with their child if they are having a general anaesthetic.
The MRI scanner is a large square machine with a deep, wide tunnel in the centre. Here is what your child will experience:
- Your child will lie on the bed. The technologist will place them in the correct position for the scan. A child having a head scan will be given a comfortable head band to wear. The head band is used to help your child keep their head in one position. They will lie with their head on a cushion which will help keep their head in a straight position. They will still be able to breathe normally but they must lie as still as possible for the whole time each scan is being done.
- When everything is ready, the bed will be moved into the tunnel. All of your child’s body will be inside the tunnel. The scanner makes a loud knocking or drumming sound during scanning. Everyone staying in the room will wear earplugs or headphones to help reduce the noise.
- Each scan lasts one to 10 minutes. You can speak to your child between scans, but it is very important for your child to hold still during this time. The technologist will talk to you and your child through a speaker. When the MRI study is complete, the technologist will help your child off the table.
Your child will not feel anything but they will hear a loud hammering or drumming noise. The noises they will hear will seem random and inconsistent, and interspersed with quiet periods. Your child will be given ear plugs but they will not totally reduce the noise. The technician will not be able to warn your child about when the noises will occur.
What happens after the MRI?
If your child has had sedation or general anaesthetic, you must stay until they are awake. The MRI nurse will let you know when you can leave. A radiologist will review the MRI study, and a report will be sent to your doctor. Your doctor will discuss the results of the study with you at a follow-up appointment.
If your child had a sedative, they may be sleepy, grumpy, and unsteady for four to six hours. Please check on your child carefully for about six hours after the test. Give your child only small sips of clear liquids such as water or apple juice. Your child may have a regular meal if they feel like eating. When your child is fully awake, they may return to their usual activities.
Other types of MRIs
Functional magnetic resonance imaging (fMRI)
This is a newer procedure that measures tiny changes in the brain. We know the general areas in the brain where functions such as memory, speech, and sensations are controlled. However, these areas are slightly different in every person. Also, injuries or diseases such as brain tumours can also cause the functions to move slightly to different parts of the brain. fMRI can help doctors see exactly where these important functions are taking place. This information is important for planning surgery, radiation therapy, or other treatments.
Magnetic resonance angiography (MRA)
The MRA is able to show the movement of flowing blood. This scan is used together with MRI when there is a concern about the tumour causing the blood vessels to narrow, as this can lead to a stroke.
What is the difference between a CT scan and MRI?
A CT is a type of X-ray, while an MRI uses strong magnetic fields and radio waves to produce an image.
Either computerized tomography (CT) or magnetic resonance imaging (MRI) may have been used initially to diagnose a brain tumour, when it was unknown what was causing the symptoms. However, in general, an MRI study is the most useful type of scan to look at the brain and spine (central nervous system). If available, an MRI is probably more likely to be used for repeat scans once a tumour has been confirmed. A CT scan is faster, and general anaesthesia is most often avoidable. Therefore, a CT scan may be needed in emergency situations, i.e., to rule out hydrocephalus or acute hemorrhage.