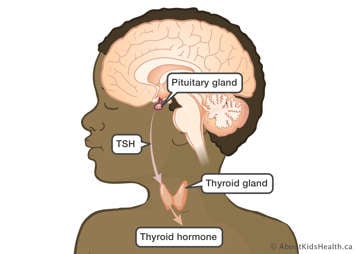
The thyroid is a butterfly-shaped gland located in the neck that produces thyroid hormone. It is controlled by a signal from the pituitary gland called thyroid stimulating hormone (TSH). Rarely, tumours near the pituitary gland impact the production of TSH, which consequently impacts the thyroid gland.
More commonly, abnormal function of the thyroid gland itself follows radiation treatment involving the brain and/or the spine. Radiation can lead to decreased thyroid function (hypothyroidism) or increased thyroid function (hyperthyroidism).
Thyroid hormone affects many important processes in the body that regulate energy. For example, thyroid hormone controls how our bodies use oxygen and break down carbohydrates and cholesterol from food. It can also impact growth.
What are the symptoms of thyroid problems?
When thyroid hormone levels are low (hypothyroidism), body functions may slow down. The symptoms can be very subtle, or very obvious. Some of the symptoms of hypothyroidism include:
- poor growth
- abnormal menstrual cycles
- fatigue
- weakness
- dry skin
- constipation
In contrast to hypothyroidism, overactive thyroid gland (hyperthyroidism) occurs very infrequently after radiation therapy. Symptoms of hyperthyroidism include:
- anxiety
- palpitations (rapid heart rate)
- weight loss
- difficulty falling asleep
- trouble concentrating in school
What causes thyroid problems?
A brain tumour or radiation therapy may cause thyroid problems in one of two ways:
- The brain tumour and/or radiation to the brain may damage the pituitary gland, which produces TSH, the hormone that controls the thyroid gland. When the pituitary gland is damaged by radiation or by the tumour, TSH production may decrease. As a result, the production of thyroid hormones will also decrease or stop.
- During craniospinal radiation, the radiation beam may exit the body near the thyroid gland. This may cause damage to the thyroid gland itself. As a result, the gland may not be able to produce enough thyroid hormone. This may push the pituitary gland to make more TSH to try to increase thyroid hormone production, although this may still not be enough.
How will thyroid problems be assessed?
At lease once per year, during clinic visits, the doctor or nurse practitioner will ask if there are any symptoms suggesting abnormalities in thyroid function. TSH will be checked in blood tests. Height will be measured and recorded on a growth chart.
How can thyroid problems be treated?
Low thyroid hormone levels, hypothyroidism, can be replaced with synthetic thyroid hormone called levothyroxine (Synthroid, Eltroxin). It is taken daily in a pill form. The decision to recommend this may be made by the treatment team and an endocrinologist, a doctor who specializes in treating hormone problems.
Individuals with overactive thyroid, hyperthyroidism, may take a medication called methimazole to decrease the function of the thyroid gland.
How will thyroid problems affect your child’s future?
Children who are affected by hypothyroidism will need lifelong thyroid hormone replacement.
Thyroid problems can develop 10 or more years after treatment, so thyroid hormone levels should be checked each year for life for children at risk of thyroid function problems. This is particularly important prior to and after becoming pregnant, as thyroid requirements change during pregnancy.
Thyroid nodules
Radiation treatment can occasionally cause abnormalities in cells outside of the tissue being targeted (the tumour). These cell changes may lead to the development of growths. Radiation involving the thyroid gland can lead to thyroid nodules (growths). Nodules may be either benign (non-cancerous) or malignant (cancerous). The risk of developing thyroid nodules depends on the amount of radiation delivered to the thyroid gland.
At each clinic visit, the doctor or nurse practitioner will feel the thyroid gland for lumps. They may recommend an ultrasound of the thyroid gland. If the ultrasound shows concerning changes, a needle biopsy may be suggested to obtain a sample of cells from the thyroid. This is performed during a brief visit to the hospital and does not require an overnight stay.
Not all thyroid nodules require intervention, however, when treatment is needed, both benign and malignant thyroid nodules are generally very treatable with surgery.
Thyroid nodules may develop years or decades after brain tumour therapy, so it is important to continue yearly checks.
