Before your child’s blood and marrow transplant (BMT), doctors need to collect stem cells from the donor. There are two ways a donor can give stem cells. They can donate cells from their:
- bone marrow. This is called a bone marrow harvest.
- peripheral blood. This is called a peripheral blood harvest. Parent donors give stem cells from the peripheral blood.
The donors can be unrelated or related to your child. In some cases, the donor will be a sibling.
Bone marrow harvest
A staff transplant physician together with another BMT fellow will perform the bone marrow harvest.
The procedure usually takes place in an operating room and takes about one to two hours.
In many cases, siblings are donors. As a parent, staying calm will help your child who is donating before the harvest. The medical team will ensure the process is as comfortable as possible.
To take bone marrow cells:
- The donor will be given a general anaesthetic so they will not be awake during the procedure.
- Both sides of the hips will be scrubbed with a disinfectant and the surrounding area covered or draped with sterile sheets.
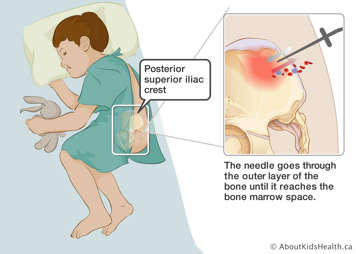
- The doctor inserts a needle through the skin until it touches the top of the hip bone, called the posterior superior iliac crest. This is the largest and uppermost bone in the pelvis and contains a large amount of bone marrow.
- Once the needle touches the hip bone, the doctor pushes the needle through the hard outer layer of the hip bone and into the bone marrow space.
- A syringe is then attached to the needle to draw out a small amount of the red liquid bone marrow. The physicians do multiple injections to collect enough of the bone marrow.
After the procedure
The bone marrow site may be sore for a few days. There may also be a bruise on the site, which will not take too long to heal. To help relieve the pain:
- Apply ice packs to the site.
- Take pain medicine, which the doctor can prescribe.
If the BMT physicians withdrew a lot of bone marrow, they may prescribe an oral iron supplement.
What complications can occur?
Bone marrow harvesting is generally a safe procedure. While the donor may feel mildly sore for up to one to two days following the procedure, serious complications rarely occur. Sometimes problems occur at the site where the bone marrow cells were taken. These include:
- bleeding: There is a higher chance of this happening with children who have pre-existing bleeding problems. In this case, the physician will order platelet and/or plasma transfusions before the test to prevent any bleeding that might occur. If bleeding does occur, the nurse will put pressure on site and monitor closely.
- infection: If the skin or bone becomes infected and is painful, or there is redness and swelling, the doctor may prescribe antibiotics through an IV or by mouth.
If any of the following symptoms occur, call your doctor right away:
- more tenderness, pain, redness, or swelling at the biopsy site
- a fever
- bleeding or drainage, such as pus, from the biopsy site. If bleeding occurs, place pressure on the site and call your doctor.
Peripheral blood stem cell harvest
Parent donors will donate their stem cells via a peripheral blood stem cell harvest. Only half of the parent’s HLA antigens match their child’s tissue. This is called a haplo-identical match.
Before the harvest
Three to five days before the harvest, you will take daily injections of a synthetic protein called filgrastim (G-CSF or granulocyte colony stimulating factor). The protein helps moves the blood stem cells from the bone marrow space into the blood stream.
The doctor will also insert a new temporary central venous line (CVL) into your femoral vein, which is the large vein in the thigh. This is called a femoral line catheter.
During the procedure
- Blood is withdrawn from your CVL. In addition to stem cells, the blood contains many other types of cells, such as red blood cells, platelets, and white blood cells.
- Your blood runs through the flexible tubing which is attached to a machine that separates out blood cells. This is called an apheresis machine. It separates the stem cells, while returning the rest of the blood back into your body. The entire procedure usually takes about four hours to complete.
- The stem cells are mixed with a preservative called dimethylsulfoxide or DMSO. The cells are then frozen at very low temperatures (cryopreserved), until the day of your child’s transplant.
How will the donor feel during the harvest?
During the stem cell harvest, the donor may feel:
- light headed
- cold
- numb around the lips
- cramps in the hands. This is caused by a blood-thinning drug that lowers the calcium level in the blood. If the cramping continues after the harvesting, calcium supplements can help.
After the stem cell harvest
Once your stem cells have been collected, they are sent to a lab for further processing.
In addition to stem cells, peripheral blood also contains a type of white blood cell called T-cells. Only half of your HLA antigens match your child’s tissue. This is called a haplo-identical match. Because this is a significant HLA mismatch, we need to process the peripheral blood to take out unwanted T-cells, so the final product just contains stem cells. Lab specialists do this using a technique called CD34 selection.
CD34 selection
Stem cells have a special protein on their surface called CD34. The lab technicians filter the peripheral blood sample through a machine which separates cells. This machine selects cells with CD34 on their surface (and hence selects for stem cells). Once purified, the stem cells are frozen at very low temperatures (cryopreserved), until the day of your child’s transplant.