Veno-Occlusive disease (VOD) is an uncommon, but serious liver problem. In VOD, the blood vessels that transport blood through the liver become inflamed and blocked. This causes the liver to swell. Because of the lack of blood supply, the liver cannot remove toxins, drugs and other waste products from the blood, which is one of the liver’s essential functions. Eventually, fluids build up inside the liver, making it more tender. The kidneys may keep excess water and salt, causing the arms, legs and abdomen to swell.
In most cases, VOD is not severe, and the damage to the liver can be reversed. But serious VOD can be life-threatening. In this case, extra fluid in the abdomen puts pressure on the lungs, making it difficult to breath.
What causes VOD?
VOD is uncommon, but usually occurs if your child has received extensive high-dose chemotherapy and/or radiation.
Symptoms of VOD
Signs that your child may have VOD usually develop one to four weeks after he starts preparing for his transplant. The symptoms include:
- jaundice, which causes the skin to yellow
- an enlarged liver
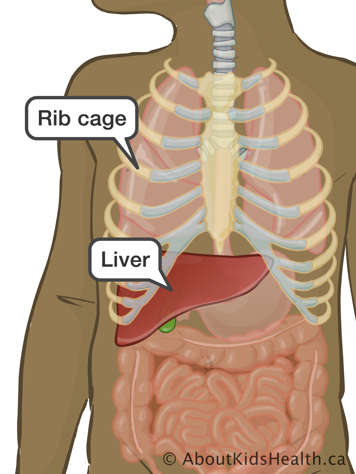
- pain or tenderness in the liver, which is located on the right side of the body under the lower rib cage
- gaining weight, quickly
- swelling of arms, legs, and abdomen. This is called edema
- fluid accumulating inside the abdomen, which is called ascites
However, a lot of these symptoms may be signs of liver disorders other than VOD. If your child experiences one or a combination of these symptoms, the doctor will perform necessary tests to find out what may be the cause.
Soon after the transplant, some children develop all of the following:
- An enlarged liver
- Sudden weight gain
- Jaundice
If doctors do not find any other causes for these symptoms, then the child most likely has VOD.
Treating VOD
Doctors will give your child medicines to control the pain, such as morphine which is given intravenously (IV). Your child’s doctor may also do a liver biopsy to get a better picture of the damage to your child’s liver.
To reduce the damage to the liver, your child’s health care team will balance the amount of fluid and/or perform abdominocentesis.
Balancing the amount of fluid
To help the liver heal, your child’s doctor carefully balances how much fluid your child intakes with how much he loses through urine. This is usually done by giving your child a limited amount of fluid to drink. At the same time, the doctor will monitor how much fluid your child loses through urine. Balancing the amount of fluid in your child ensures that we do not cause severe dehydration.
Abdominocentesis
In severe cases of VOD, your child’s doctor may drain any extra fluid in the abdomen. This is done through a procedure called abdominocentesis, in which doctors use a hollow needle to draw out fluid from the belly.