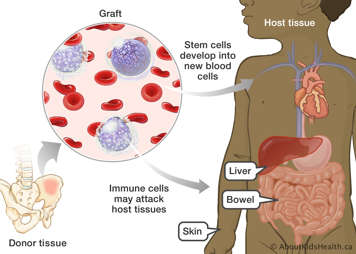
After an allogeneic blood and marrow transplant (BMT), some children may develop a common complication, called graft vs host disease (GVHD).
GVHD occurs when the new bone marrow stem cells, called the graft, recognize your child (the host) as different from what they expect. The graft contains donor white blood cells called lymphocytes, which distinguish between cells that belong in the body and those that do not. During GVHD, the graft sends out lymphocytes to attack your child’s organs and tissues. The new stem cells can damage organs such as the liver, skin or bowel.
Receiving stem cells from an unrelated or mismatched HLA donor increases your child’s chances of developing GVHD.
There are two types of GVHD: acute GVHD and chronic GVHD. Your child may develop one, both or neither.
- If GVHD develops early (often within three months) after transplant, it is called acute GVHD.
- If GVHD develops later after the transplant, it is called chronic GVHD. Compared to the acute form, chronic GVHD can affect many more organs and cause life-long scarring (for example, on the skin).
Symptoms of acute GVHD
Common signs of GVHD include:
- skin rash, usually starts on the palms or feet but may be on the chest or back. In severe cases, the rash may spread to other parts of the body and become redder in colour (similar to sunburn).
- diarrhea
Signs that GVHD is affecting the liver include:
- yellowing of the skin and eyes (jaundice)
- mild liver tenderness
- increased amounts of a yellow substance the body normally excretes, called bilirubin. The body gets rid of bilirubin through a fluid excreted by the liver, called bile. When there are high levels of bilirubin in the body, the bile is not working properly.
Symptoms of chronic GVHD
Some of the more common signs of chronic GVHD affect different parts of the body.
- Eyes – dryness, with increased tearing and redness
- Mouth – dryness with ulcers or sores and changes in taste
- Skin – areas of decreased and increased colour, scarring and thickness. This can cause tightness across joints
- Gut – changes in appetite, frequent loose stools, and unable to gain weight
Treating GVHD
Children who develop GVHD usually take a combination of medicines. Since some of these medicines also prevent GVHD, your child may be given these medicines prior to the transplant. The doctor may increase the dose if your child develops GVHD after the transplant. If your child develops GVHD of the bowel (gut GVHD), the doctor may need to put them on a specialised diet. This diet will help your child’s bowel rest and heal.
Prednisone
Prednisone helps treat and prevent GVHD by weakening your child’s new immune system. This way, the new immune system has more time to get used to and tolerate your child’s body. These types of drugs are called immunosuppressants. A healthy immune system fights off cells that do not belong in the body, such as bacteria and other tissue it does not recognize. The goal is for your new immune system (transplant) to accept your body, not attack it. This is why prednisone is the first type of drug doctor’s use to treat and prevent your child’s GVHD.
Your child may need to use prednisone for a long period of time, depending on the severity of the GVHD.
Cyclosporine
Similar to prednisone, cyclosporine is an immunosuppressant. It both prevents and treats GVHD. All children who receive stem cells or bone marrow from a donor will start on cyclosporine before their transplant date. During the transplant period, the doctor needs to make sure your child is receiving an adequate amount of cyclosporine. They will check the level of cyclosporine in your child’s blood periodically.
Your child continues to take cyclosporine for about six months after the transplant. After being discharged from the hospital, a nurse will check your child’s cyclosporine levels every week.
Methotrexate
Methotrexate stops the cells from dividing and making new cells. Methotrexate is used to prevent GVHD following bone marrow or stem cell transplant. Children who receive stem cells or bone marrow from a donor may receive three or four doses of a methotrexate. Since this medicine may cause mouth sores, good mouth care is very important.
For more information, please see Daily Care.
How long will your child have GVHD?
If your child gets GVHD during treatment, the disease usually subsides in a month or two. Chronic GVHD often starts more slowly and takes longer to respond to treatment. Depending on your child’s response to the first medication, doctors may need to use other medicines to control chronic GVHD.