
What is esophageal atresia or tracheoesophageal fistula (EA/TEF) repair?
EA/TEF repair is surgery within the first few days of life to correct defects in the esophagus, the tube leading from the mouth to the stomach.
How might EA/TEF repair affect my child’s eating and drinking?
After an EA/TEF repair, your child may find it difficult to swallow food and liquids (including their own saliva). This difficulty is called dysphagia. Some children require a feeding tube to support their nutrition while working towards taking full feeds by mouth.
Causes of dysphagia
- Dysphagia can occur if the muscles and nerves of the esophagus have difficulty co-ordinating themselves. This makes it more difficult for food and liquids to move towards the stomach.
- Sometimes food and liquid can collect in the esophagus at the site of the surgery. This can stretch the upper portion of the esophagus If this happens, your child is at higher risk of choking.
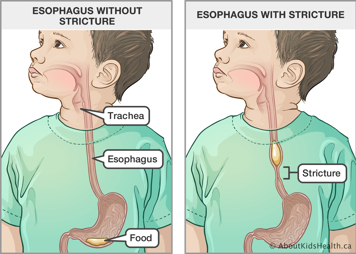
- Scar tissue at the surgical site may tighten. This can make the esophagus stricture (become narrower), making it difficult for food and liquid to pass through the esophagus into the stomach. If you notice signs of an esophagus stricture (difficulty swallowing food, increased secretions, etc.). notify your child’s surgical team as there is a risk of aspiration due to the narrowing.
How to help your child eat after EA/TEF repair
Bottle or breastfeeding
- Your child may experience difficulties drinking liquids and may need to be assessed by an occupational therapist (OT) while in the hospital.
- If your child is having difficulty swallowing, their esophagus may have narrowed and they may require a procedure to dilate their esophagus. Contact your child’s health-care provider.
Introducing solid food to babies
- Pureed food is usually introduced to a child between four and six months of age. This will likely be the case for your child as well. Check with your child’s health-care provider before starting your child on purees.
- Once your child is able to take smooth purees without difficulty, you can gradually progress to offering thicker, more solid textures. Ensure that your child is able to sit comfortably with their head and trunk supported (e.g., in a highchair or infant seat). Contact your child’s health-care provider if you are unsure about the safety of this for your child.
Offering solids to toddlers and older children
- As your child’s diet progresses, avoid food that is sticky or gooey or food that becomes sticky or gooey after chewing, such as soft bread. This type of food can be hard to swallow because it becomes a sticky ball when it is chewed.
- Be aware that some children gag and refuse solids or lumpy food. If this is your child’s experience, ask your child’s occupational therapist (OT) for tips to help move from one food texture to another.
- If you are offering table food, make sure it is cut into small pieces and that your child chews it really well. Very hard food, or food that is not chewed well, can be difficult to swallow and may get stuck.
- Serve foods with lots of liquids (such as dressings, dips, sauces and gravies) to help with swallowing.
- Some finger and table food can help to keep scar tissue stretched, but children may tolerate some textures more than others.
Mealtimes
Mealtimes should be similar to those for any child.
- Provide a balanced diet that includes all food groups from Canada’s Food Guide: vegetables and fruit, grain products and protein foods.
- Serve your child several small meals during the day. Many children need to eat five or six small meals throughout the day after esophageal atresia or tracheoesophageal fistula (EA/TEF) repair.
- Aim for meals every three or four hours.
- Follow your child’s cues (e.g., stopping if your child is disinterested or fatigued). Do not let mealtimes last more than 30 minutes.
- Encourage your child to:
- sit upright while eating (highchairs or booster seats can help younger children)
- take small bites and chew their food well
- eat slowly
- If your child wants to eat quickly, you may need to limit how much food is on their plate. Allow them to fully chew and swallow before giving them more.
- If your child finds it difficult to eat within the time limits of school meal or snack times, talk to your health-care provider about offering higher calorie drinks (such as smoothies or yogurt drinks).
How to deal with common swallowing problems
Food getting stuck
Sometimes food will get stuck in the esophagus for a short time. In most cases, it will slowly pass through or your child will cough it up.
- To prevent food from sticking, let your child take a few sips of liquid after every two or three bites.
- Add more dressings, dips, sauces or gravy to food to help your child swallow it more easily.
- If food does get stuck, stay calm and offer a few sips of liquid.
- Suggest that your child sing their favourite song or ask your child simple questions to help stay calm while they wait for the food to go down.
- If an item remains stuck, contact your health-care provider. Call 911 if your child is turning blue, having trouble breathing or making abnormal sounds that are not going away.
Inability to eat or drink because of strictures
- If your child’s esophagus develops a stricture (a narrowing caused by scar tissue), they may not be able to eat or drink. Their esophagus will need to be dilated (stretched). In the meantime, your child’s health-care team can give you instructions to care for your child.
- If your child can still take liquids by mouth, you will be instructed on how to keep them hydrated.
- If your child has a feeding tube, you will be instructed to give formula or fluids through the tube.
- If your child cannot tolerate any liquids or solids or has signs or symptoms of choking or difficulty breathing, please bring your child to the Emergency Department for assessment.
When to get medical help for swallowing difficulties
Contact your child’s healthcare provider if:
- your child is struggling to swallow solids, liquids or their own saliva
- food has gotten stuck and does not pass through with the help of some sips of liquid
- your child’s eating has changed significantly (only liquids or gagging on or vomiting food) for two meals in a row
If you have concerns that cannot wait (e.g., your child is having shortness of breath or unable to tolerate any food/liquid), please go to the nearest Emergency Department for assessment.