What is a liver biopsy?
A liver biopsy is a procedure done to obtain a small sample of the liver so it can be examined under a microscope. A liver biopsy can help your child’s health-care team identify problems in the liver, find the cause of liver disease, and/or determine how much damage is in the liver.
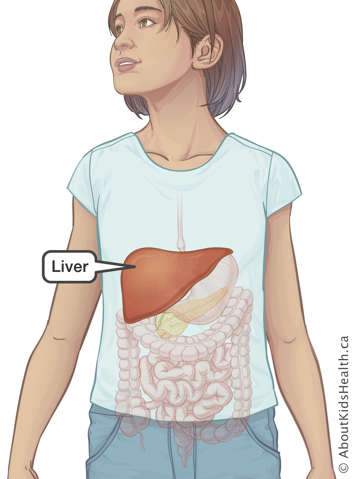
What is the liver?
The liver is an organ in our belly (abdomen). It helps our bodies remove toxins and waste. It also stores some of the energy we get from food and also helps with food digestion by producing bile fluids. The bile helps with digestion of fat from food.
What are the risks of a liver biopsy?
Liver biopsy is considered a safe procedure with only small risks, which include:
- tenderness and/or mild pain at the biopsy site
- bleeding in the liver
- injury to another organ close to the liver (lung or gallbladder)
- problems with sedation or anaesthesia (please let your child’s health-care team know if your child has ever had problems with any type of anaesthesia before)
- infection at the biopsy site or in the abdomen
- leaking of bile fluid
- abnormal connection between arteries and veins in the liver as a result of the healing process after biopsy.
Risks vary depending on your child’s condition, age, and health. You should discuss any concerns you may have with your child's health-care provider.
Some medications, diet supplements or herbs may increase the risk of bleeding from liver biopsy. Please discuss all medications, supplements, and herbs that your child is taking with your the health-care team. If you are unsure, bring all of your child’s medication, supplements, and herbs—including over-the-counter medications—with you at your pre-procedure appointment.
How to prepare for liver biopsy
Clinic visit to prepare for liver biopsy (pre-procedure appointment)
The interventional radiologist and their team will see most children for assessment a day or two before the procedure. During the clinic visit you should expect:
- a physical health assessment and blood work to make sure that your child is healthy and that it is safe to have local anaesthesia, sedation or general anaesthesia.
- an overview of the procedure, and a review of the consent form with an interventional radiologist.
- a quick ultrasound of the liver to locate the biopsy site; it will be then marked with a semi-permanent marker on your child's abdomen.
In some cases, your child may need to be admitted to hospital before having a liver biopsy. Your child’s health-care team will give you specific instructions about where you need to take your child before the liver biopsy.
Giving consent before the procedure
Before the procedure, the interventional radiologist will:
- explain how and why the procedure is done
- the potential benefits and risks
- discuss what will be done to reduce these risks
- help you weigh the potential benefit of the procedure against any risk it may pose for your child.
Signing the consent form means you agree to the procedure. Before you do so you should understand all the risks and potential benefits of the liver biopsy. Make sure you get answers to all your questions. A parent or legal guardian must sign the consent form for children who are not able to give consent.
The procedure will not be performed unless you give your consent.
How to prepare your child for the procedure
You should talk to your child about what will happen before any treatment. Children feel less anxious and scared when they know what to expect. Children also feel less worried when they see their parents are calm and supportive.
When talking to your child, use words they can understand. Let your child know that they will receive medicines to make them feel comfortable during the procedure.
If your child becomes ill within two days before the procedure
For their own safety, it is important that your child is healthy on the day of the procedure. If your child starts to feel unwell or has a fever within two days before the liver biopsy, let the health-care provider who ordered the biopsy know. Your child’s procedure may need to be rebooked.
Food, drink and medicines before the procedure
Your child’s stomach must be empty before sedation or general anaesthetic. Thus, on the day of the liver biopsy, your child will have to fast (stop eating and drinking) several hours before the procedure. The length of time required for fasting will depend on your child’s diet and the type of food and drink consumed. Your child’s health-care team will give you specific instructions about fasting.
Please follow the fasting guidelines carefully because it is unsafe for your child to have sedation or anaesthesia if they have eaten or had anything to drink too close to the procedure time.
If your child has special needs during fasting, talk to your child’s health-care team to make a plan.
Your child can take their regular morning medicine with a sip of water up to two hours before the procedure.
Medicines such as acetylsalicylic acid (ASA), naproxen, ibuprofen, warfarin, or enoxaparin may increase the risk of bleeding. If your child is taking any of these medicines, please discuss this with your child’s health-care provider and the interventional radiologist to make a plan for the time of the procedure.
On the day of the liver biopsy
Arrive at the hospital well before the planned time of your child’s procedure. Follow your hospital’s directives.
There, your child will be dressed in a hospital gown, weighed, and a nurse will make sure your child is healthy enough to have the procedure.
You will also be able to speak to the interventional radiologist who will be doing the liver biopsy, and the nurse or anaesthetist who will be giving your child anaesthetic or sedation.
During the liver biopsy, you will be asked to wait in a waiting room.
Your child will have medicine for pain
Children are given medicine for treatments that may be frightening, uncomfortable, or painful. This includes local anaesthesia, sedation or general anaesthesia. The type of medicine that your child will have for the procedure will depend on your child’s condition.
Feel free to discuss your questions or concerns with your health-care team.
How is a liver biopsy performed?
Your child’s health-care provider will discuss with you the best way for your child to have a liver biopsy before arranging the procedure. The approach to your child’s liver biopsy will be determined by a number of factors, including how well your child feels and the type of liver problem that the health-care team suspects.
The procedure usually takes about one hour.
Anaesthesia
Right before the procedure, your child will receive local anaesthesia (“freezing”). This means that only a specific, limited area of your child’s abdomen (belly) will be numbed so they will not feel pain from the biopsy. They may also receive sedation or general anaesthesia, which will make your child sleep or feel sleepy throughout the procedure and prevent them from feeling pain during the biopsy.
Image guided procedure
In most cases, an interventional radiologist carries out the liver biopsy using image guidance. The interventional radiologist uses an ultrasound machine to precisely locate the liver and help identify the biopsy site.
After cleaning the skin, the interventional radiologist inserts a hollow needle through the skin into the liver and then the biopsy device is inserted into the hollow needle and quickly withdrawn. This removes a tiny liver sample. Two to three samples are usually taken by re-inserting the biopsy device through the needle. The samples will then be sent to the lab for examination under a microscope.
The small hole made by the needle may bleed. The interventional radiologist puts a small plug in to stop the bleeding. The plug does not need to be removed; it will disappear on its own. A small bandage will be placed over the biopsy site. No stitches are needed.
Other image-guided biopsy procedures
In some special cases, such as when children have blood clotting problems or fluid in their belly, the interventional radiologist will instead perform a transvenous liver biopsy. This is done by inserting a small tube through a vein in your child’s neck and pushing it all the way to your child’s liver to take a small sample of liver tissue. This procedure limits the risk of bleeding.
After the procedure
After the liver biopsy is complete, the interventional radiologist will talk to you about the details of the procedure. Your child will be moved to the recovery area. As soon as your child starts to wake up, a nurse will come and get you so you can be with them.
Your child will be observed closely until they can safely go home. The time of discharge is usually between six and 24 hours. It differs depending on the age and health of the child, and the reason for the biopsy.
Your child will have a blood test about four hours after the biopsy to check for a change in blood counts and make sure the liver is not bleeding. An ultrasound scan may be ordered. Your child may have to stay on bed rest or be admitted overnight for further observation if their health-care team feels it is necessary.
Going home
Most children older than one year of age who have a liver biopsy go home the same day.
Babies under one year of age and children who are or become unwell may need to be admitted to hospital after the procedure.
Follow your health-care team’s instructions to care for your child at home.
How soon after biopsy will results from the test be available?
Results are usually available within a week but some special tests may take longer. Your child’s health-care team will be able to tell you when to expect your child’s results. Your child’s health-care provider will receive the results of your child's biopsy. You will need to make a follow-up appointment with them to discuss the results.
At SickKids
If you have any concerns in the first 48 hours, call the Image Guided Therapy (IGT) clinic at (416) 813-7654 ext. 201804. Speak to the IGT clinic nurse during working hours or leave a non-urgent message.
If you have concerns and it is after working hours, see your child’s health-care provider or go to the nearest Emergency Department. You can also call the Hospital for Sick Children switchboard at (416) 813-7500 and ask them to page a member of your child’s health-care team or the interventional radiology fellow on call.
On the day of the liver biopsy, SickKids’ staff asks that you come two hours before the procedure.
For more information on fasting see Eating and drinking before surgery.
For more information on preparing your child for their procedure see Coming for surgery.