What are G and GJ tubes?
Gastrostomy tubes (G tubes) and gastrojejunostomy tubes (GJ tubes) are feeding devices. A G tube gives liquid nutrition, medication and other fluids directly into the stomach. A GJ tube gives liquid nutrition, medication and other fluids directly into the small intestine (the jejunum). Both G tubes and GJ tubes are placed through a small opening in the stomach. This opening is called a "stoma". The tunnel from the outside of the body to the stomach is called the "tract".
Why does your child need a feeding tube?
Feeding tubes are placed for many reasons. The most common reason children need a feeding tube is to get the nutrition that they need to grow because they cannot eat and drink enough or at all. It is important to know why a feeding tube is being recommended for your child. If you are uncertain why your child needs a feeding tube, discuss this with your child’s health-care team.
Making an informed decision
The decision to get a feeding tube for your child is very personal and often difficult. However, keep in mind that you did not cause your child’s illness or feeding difficulties.
Some children may need a feeding tube their whole life. Others may only need a feeding tube for a set period of time, after which the tube can be removed. Your child’s pediatrician or primary health-care team will decide what is best for your child based on your child’s medical history and general health.
If you ever decide that the feeding tube is not a good choice for your child and family, it can be removed.
Ask your health-care team for information
You are not alone. Your health-care team will support you through this decision. You can ask your team members anything. The G tube team will decide if it is safe and technically possible to insert a feeding tube. Together with your health-care team and the G tube team, you will:
- discuss the procedure, its benefits and risks, and alternatives
- prepare you and your child for the admission to hospital for the tube insertion
- learn to monitor and manage complications and challenges, as well as how to care for your child’s skin and tube at home
Take time to think about what tube feeding means for your child and family before you make the decision.
Acknowledging your feelings
Many families feel overwhelmed with this decision and what this will mean for their lives. This normal reaction triggers many feelings for families, such as:
- fear
- worry
- guilt
- disappointment
- feelings of failure
- upset about giving up "normal" feeding
Your feelings are important. Let your child’s health-care team know how you feel. The health-care team will do its best to help you and your child identify and acknowledge your feelings and come to terms with your decision.
Benefits to having a feeding tube inserted
If it is safe to feed your child by mouth, they will still be able to enjoy eating and drinking my mouth despite having a feeding tube. The feeding tube will give extra nutrition in addition to what they will take by mouth.
A feeding tube can provide the following benefits:
- optimize nutrition and hydration
- better growth and brain development
- easier way to give fluids, especially when sick
- easier way to give medications, especially those that taste bad
- decreased stress and time for feeding by mouth
- ability to let gas out of your child’s stomach when bloated (this is like artificially burping your child; this benefit applies only to G tubes, not GJ tubes)
- fewer hospitalizations and emergency room visits
- safer feeding, more discreet and comfortable than a nasogastric (NG) tube
Children with feeding tubes can still do all of the activities (including swimming) that they may have done before the tube was inserted. They may even have more energy and be more active.
Challenges you may face with a feeding tube
Despite the many benefits to having a feeding tube, taking care of it can be time-consuming, affect your lifestyle, and seem overwhelming.
Familiarize yourself with day-to-day feeding tube care. Daily, you will have to:
- give your child feeds
- safely store and handle your child’s feeds
- clean the equipment
- clean and care for the feeding tube site (stoma and surrounding skin)
- know, watch for, and manage all possible complications
There are costs to having and maintaining a feeding tube. You will have to buy supplies for the feeding tube. You may also need to purchase a feeding pump. Ask your health-care team about financial supports to help you with your costs.
Limitations of each type of tube
G tubes
- Some G tubes can only be changed in an Interventional Radiology department in a hospital. Some can be changed in a clinic or by the family.
- Small sized tubes may block easily.
- Your child may have skin irritation from the tube being taped to the tummy.
- The tube may be accidently pulled out.
- The feeding tube site can become infected, leak or develop granulation tissue.
- For most children, replacing an NG tube with a G tube improves reflux, but this never eliminates reflux. For some children, it may even get worse.
GJ tubes
- GJ tubes have the same risks as G tubes and have other issues.
- GJ tubes increase the risk of intussusception (when one part of the bowel slips into the next part).
- GJ tubes can only be changed under image guidance in the hospital.
- Feeds must be continuously delivered with a pump.
- There are higher risks of the tube moving into a place it is not meant to be (tube migration).
Getting support
You will learn how to take care of your child’s feeding tube before you go home. The Connected Care Program at SickKids offers you personalized teaching tailored to your child’s specific needs, ensuring you are confident in managing the tube feeds at home. Not only will they provide you the education, they will review with you the resources/supplies you will need and provide ongoing support for home. Ask questions, especially if you do not understand what is required in day-to-day feeding tube care. You can also reach out to the team or other parents/caregivers for support.
It is important that all of your child’s caregivers (including babysitters and other family members) are taught to safely care for the tube. You may be able to get some support from homecare nurses but most of the responsibility to look after your child’s tube will be yours and your family’s. Looking after a child with a G or GJ tube will be an adjustment. With time, however, you will become comfortable with the feeding tube and it will become a part of your daily routine.
Making the decision
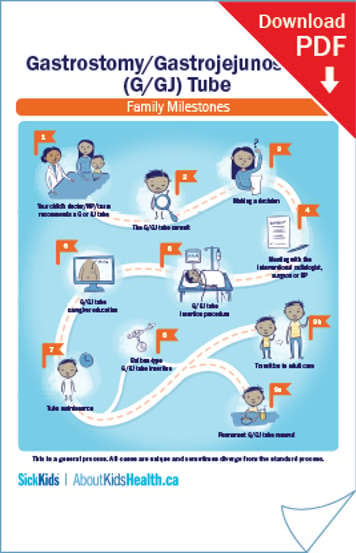
This PDF outlines the general steps you can expect if your child receives a G or GJ tube. Use it to learn more about the process and/or write down any questions or notes.
Most families are glad they made a decision to get a G or GJ tube for their child. Although there may be challenges along the way, families adjust either on their own or with the help of their health-care provider.
Some families decide not to proceed with a G or GJ tube for their child because it was just not the right option for their child and family.
Ultimately the decision to get a G or GJ tube for your child is yours. But you do not need to make it alone. Talk to your family before making the decision.
The health-care team will answer your questions and help you make a decision that is best for your child.