What is diaphragmatic pacing?
Diaphragmatic pacing is another way to provide mechanical ventilation. It uses your child’s diaphragm as a ventilator and is for children who have normal lungs and a normal diaphragm and phrenic nerve (nerve that controls the diaphragm).
To receive diaphragmatic pacing, your child will need surgery to have electrodes and receivers placed near their diaphragm. After the surgery, your child will have a short healing period before diaphragmatic pacing starts.
Your child's healthcare team will decide your child's initial diaphragmatic pacing settings and make ongoing adjustments Do not change anything without checking with the team.
How does diaphragmatic pacing work?
- An external unit called a pacing transmitter stimulates an electrode sitting underneath your child’s phrenic nerve.
- In turn, the electrode sends an electrical pulse to the phrenic nerve.
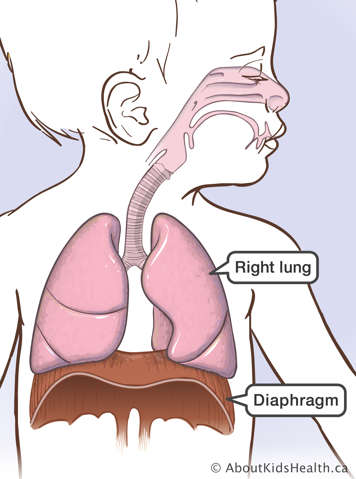
- This causes the diaphragm to contract and move downwards, allowing air to move into the lungs.
- When the electrical pulse stops, the diaphragm relaxes and moves upwards, causing air to leave the lungs.
Your child’s doctor can change your child's diaphragmatic pacing settings with the pacing transmitter to make sure your child receives enough ventilation support.
Who can use diaphragmatic pacing?
- Children who need mechanical ventilation throughout the day and night may use diaphragmatic pacing to improve mobility and quality of life during the day.
- Children who are ventilated only at night may use diaphragmatic pacing as an alternative method of ventilation. Children who are using a tracheostomy and a ventilator before starting diaphragmatic pacing may ultimately be able to have their tracheostomy tube removed.
- Patients with congenital central hypoventilation syndrome (CCHS) or certain spinal cord injuries might also benefit from diaphragmatic pacing.
Restrictions on diaphragmatic pacing
Diaphragm pacing is not suitable for everyone or suitable 24 hours a day.
- Because the diaphragm gets tired, pacing can only be used 12 to 16 hours a day.
- Pacing should only be considered when a child’s diaphragm and phrenic nerve are intact.
- A child cannot receive pacing if they have a neuromuscular disease (such as spinal muscular atrophy or Duchenne muscular dystrophy).
- Pacing works best for children that are at least three years old. In younger children, pacing can increase the risk of airway collapse.
What are the possible complications of using a diaphragmatic pacer?
- Your child may experience sharp pain in their shoulder when pacing is started. This typically indicates that there is over-stimulation and the healthcare team needs to adjust the tidal volume setting.
- Some children may twist their receivers underneath the skin, causing a twist in the electrode lead wire.
- Because the receiver and electrode are implanted during surgery, there is a small risk of infection. If your child has a fever with an unknown cause, please call your doctor immediately.
- Diaphragmatic pacing can cause upper airway collapse. Decreasing the tidal volume lowers this risk. Please let your child's healthcare team know if you suspect upper airway collapse, for example if your child is snoring, experiences increased effort to breathe at night or has stridor (a high pitched, harsh sound when they breathe).