What is hypopituitarism?
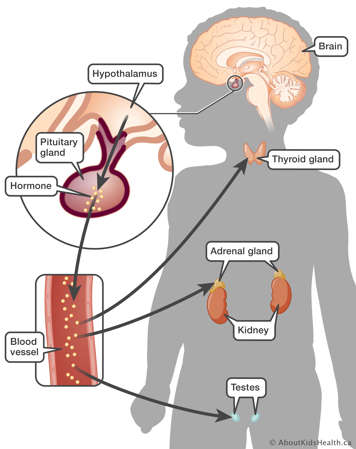
Hormones are chemicals produced in the body. They act as messengers that travel to other parts of the body where they affect how organs work. Hypopituitarism is a condition where the pituitary gland does not produce one or more pituitary hormones, or it does not produce enough hormones. “Hypo” means less than usual. The term "panhypopituitarism" means many or all of these hormones are deficient ("pan" means all).
The pituitary is a pea-sized gland located in the middle of the skull. It is part of the body’s endocrine system, which includes all of the glands that produce and regulate hormones. The pituitary gland acts as the control centre for other glands. Hormones produced in the pituitary gland impact many other parts of the body. The pituitary releases various hormones in response to chemical messages it receives from the part of the brain called the hypothalamus.
What is gonadotropin?
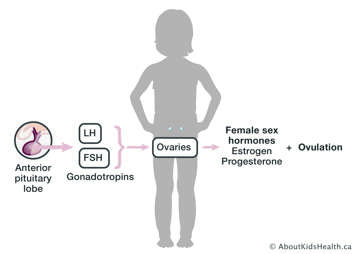
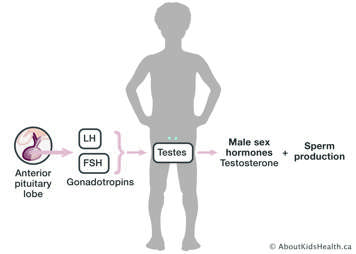
The hormones made by the pituitary gland that begin the process of pubertal development are called gonadotropins. The main gonadotropins are follicle stimulating hormone (FSH) and luteinizing hormone (LH).
In girls, these hormones signal to the ovaries to make primarily estrogen and progesterone, the hormones that cause breast development, ovulation, menstrual periods, and other changes including rapid growth in height and change of body shape. They also stimulate the ovaries to make a small amount of testosterone, leading to pubic hair growth and acne. Typically, puberty happens for girls between the ages of 8 and 12.
In boys, these hormones signal to the testes (testicles) to make testosterone and to begin sperm production. Testosterone is the hormone that causes increased size of the penis and testes, facial hair growth, voice deepening, and other body changes including rapid growth in height and muscle mass. Typically, puberty happens for boys between the ages of 9 and 14.
What is gonadotropin deficiency?
When children have gonadotropin deficiency, they will fail to enter puberty or may stall in their pubertal development during the teen years. If these hormones are absent, they do not need to be replaced until the child is ready to enter puberty. The sex hormones, testosterone for boys or estrogen and progesterone for girls, will be used to initiate and maintain pubertal development.
How is gonadotropin deficiency diagnosed?
Several ways your health-care provider determines if your child is unable to make adequate amounts of gonadotropin hormones are by completing and reviewing the following tests:
- physical exam
- growth rate
- bone age X-ray
- blood tests
Damage to the pituitary may cause LH/FSH to be produced too early (before age 8 in girls and age 9 in boys) causing precocious (early) puberty. It may also cause them to not be produced at all, causing delayed or absent pubertal development (no sexual development in girls by age 13 and in boys by age 14).
How is gonadotropin deficiency treated?
Treatment for girls
For girls with delayed puberty, estrogen is provided in pill (Estrace or Premarin) or transdermal (through the skin) patch form (Estradot). Estrogen therapy is started slowly to closely copy the gradual rise of estrogen that would normally take place in the body. Generally, it will take up to 2 years of estrogen treatment before progesterone is added and menstruation begins. When progesterone is added to the treatment plan, this will cause “withdrawal bleeds” or periods. Once pubertal development is complete switching to oral contraceptive pill or estrogen patch and oral progesterone is used as hormone replacement.
Effects of estrogen include:
- increases in height
- development of breast tissues
- growth of the uterus
- gradual change to a more feminine body shape
- mood changes and mood swings
- increased appetite
- improved bone mineral density
- slight changes in voice
- increased sexual interest
Spotting of menstrual blood should not occur while on estrogen alone, but if it does, contact your health-care provider. These sex hormones do not cause growth of pubic and underarm hair (which may be thin in individuals with hypopituitarism).
Estrogen pills should be stored at room temperature and protected from light and moisture. The pills should be taken in the evening, as your child may experience some nausea. The important part to remember is to be consistent and take the pills at the same time each day.
Estrogen patches are changed twice weekly and should be kept in a warm, dry place.
Treatment for boys
For boys with delayed puberty, testosterone is most often given by injection, but it is also available in creams, gels, and transdermal (through the skin) patches. Generally during the adolescent years, testosterone is given by injection (Depo-testosterone, Delatestryl) into a large muscle in the thigh or the buttock (gluteal muscle) every 2 to 4 weeks. Often these injections are given by a nurse or doctor in your local doctor’s office.
Effects of testosterone are:
- growth in height
- appearance of underarm, pubic and some body hair
- acne
- increase in the size of the penis
- beginning of penis erection and ejaculation
- increases in muscle throughout the body with a gradual change to a masculine body shape
- mood changes and mood swings
- increased appetite
- deepening voice
- increased sexual interest
Testosterone injections do not increase the size of the testes.
Important side effects to tell your child’s doctor or nurse about include having a prolonged erection, or any significant pain, swelling, or redness at the injection site.
The testosterone medicine for injection should be stored at room temperature. One vial can be used for multiple doses for up to 2 months.
Follow-up care and long-term outcomes
In both girls and boys, frequent clinic visits (every 4 to 6 months) are necessary when sex hormone treatment is started. Sometimes dose adjustments are made to ensure that these body changes are not occurring too slowly or too quickly. For the same reason, bone age X-rays of the left hand and blood tests are taken at some of these clinic visits. Once growth is completed and an appropriate dose in hormone is established, visits will move to every 6 to 12 months. Sex hormone treatment is given well into adult life. While it is not life-threatening to stop these therapies, they provide benefits to normal adult life.
As adolescents and young adults mature, they are able to experience normal sexual function. However, lack of gonadotropins will affect fertility (ability to have children). Since new developments related to fertility are constantly being explored, your child will need to consult with fertility specialists in the future when planning to have children.
Your child and their health-care team may consider whether to stop or decrease the sex hormone replacement in late adult life.
Infertility and hypopituitarism
For women
A woman without healthy ovaries is unlikely to conceive a baby naturally. A donated egg may be fertilized with her partner’s sperm and placed in her uterus.
Women who have healthy ovaries but no chemical message from the brain to the ovaries will need help in becoming pregnant. These women may be given LH/FSH by injection (prescribed by a fertility specialist) to help with conception.
While the chances that women with issues with ovarian function will become pregnant naturally are low, all sexually active women should use condoms for birth control and prevention of sexually transmitted infections.
For men
Men without healthy testes are unlikely to father a child naturally but may be able to use donor sperm to conceive a child with a female partner.
Men who have healthy testes but no chemical message from the brain to the testes will need help fathering a child. These men may be given LH/FSH by injection (prescribed by a fertility specialist) for a period of time until their partner conceives.
The possibility of fathering a child naturally without medical assistance is low but is not impossible. All sexually active men should use condoms for birth control and prevention of sexually transmitted infections.
