What is sickle cell disease (SCD)?
Sickle cell disease (SCD) is an inherited blood disorder. It is not contagious. SCD is more common in people with an African or Caribbean background, but children of Middle Eastern, Mediterranean and South Asian ancestry are also affected.

Signs and symptoms of sickle cell disease
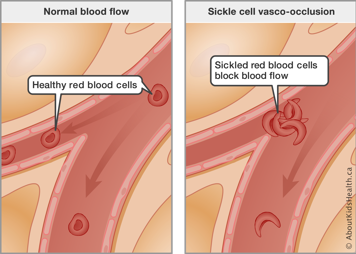
The two main characteristics of SCD are chronic (long-term) anemia and recurrent episodes of vaso-occlusion:
- Anemia is caused by a lack of either hemoglobin or red blood cells in the body. When this happens not enough oxygen gets delivered to the body and can cause paleness, tiredness or fatigue, and weakness. Sickle-shaped cells do not live as long as regular red blood cells. They die faster resulting in an increased breakdown of red blood cells. The liver sometimes cannot keep up with filtering all the broken-down cells and the bilirubin from the broken-down cells can build up in the system making the whites of the eyes appear yellow from time to time.
- Vaso-occlusive episodes are blockages of the blood vessels anywhere in the body caused by deformed red blood cells. Sickle-shaped red blood cells cannot flow through the body as well as regular red blood cells and tend to clump together. This leads to blockages and a lack of oxygen in the affected area of the body. Symptoms depend on where the blood vessels are blocked. If the blood vessel going to a leg bone is blocked, then there will be pain in the leg. If a blood vessel going to the brain is blocked, then there will be symptoms of a stroke, such as weakness on one side of the body.
Pain episodes
The most common symptom of a vaso-occlusive episode is bone pain. Any bone can be affected, including the arms, legs, back and skull. These episodes, commonly called pain crises, are unpredictable. Some children feel unwell before the actual onset of pain and can let an adult know.
Possible triggers for a pain episode include:
- infection
- stress/fatigue
- dehydration
- exposure to cold and very hot temperatures
Some pain episodes happen without a known reason.
Preventing pain episodes
As a teacher you can help to prevent a pain episode by:
- Making sure the student drinks lots of fluids so they are not dehydrated.
- Making sure the student is dressed in a few layers of warm clothing in the winter when they are going outside for recess and when they are going home.
- Encouraging parents to send an extra sweatshirt and socks to school in case the student becomes wet during recess or at any other time.
- Recognizing fever as a sign of infection and following the steps outlined below.
- Making sure the student avoids vigorous exercise without the ability to take breaks and drink fluids, especially during hot days.
Even with these measures, though, children may still have a pain episode.
What to do if your student with sickle cell disease is unwell
Temperature
- First, have the student sit or lie down in a quiet place.
- Take the student’s temperature. Caregivers are advised to keep a thermometer in the child’s bag for use at school or to leave one with the teacher for that student’s use.
- If the temperature is higher than 38°C under the armpit, or 38.5°C by mouth, call the caregivers immediately to take the student to the closest emergency department.
- Check if there is any sign of breathing problems. If yes, call an ambulance.
- If the temperature is less than 38°C and there is no sign of breathing problems then do a pain assessment.
Doing a pain assessment
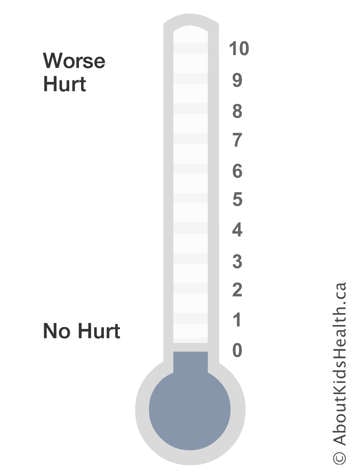
- Ask the student what level their pain is on a scale of 0 to 10, with 0 being no pain and 10 being “the worst pain ever.” Ask where the pain is located.
- If the pain is less than 7/10 and the caregivers have given the teacher or nurse a supply of pain medication, give the child a dose as prescribed by their doctor.
- If no medication is at school or if the pain is greater than 7/10, call a parent to pick up the student.
- If the pain is localized to one or two areas, a warm pack can be applied to the site of pain until the student is picked up by a parent. ICE PACKS SHOULD BE AVOIDED.
Children 5 years of age and older
Ask your student: "If 0 is no pain and 10 is the worst pain you can imagine, what are you feeling now?"
Pain management
Medications
- Before each dose, take your student's temperature. If their temperature is higher than 38°C under the armpit or 38.5°C by mouth, go to the nearest emergency department right away.
- Acetaminophen _____ mg. Repeat the dose every four hours.
- Ibuprofen _____ mg. Repeat the dose every six hours.
Physical
There are also physical strategies that your child can try to help reduce their pain. These include:
- Give your student plenty of fluids. Do not give them cold fluids.
- Encourage your student to gently massage the area.
- Apply heat to the area.
Tips for using heat
You can use heat with children three years of age and older. Do not leave young children unattended with heat.
If the area with heat applied to it becomes painful, uncomfortable or a local skin reaction develops, remove the heat immediately
To apply heat you can:
- Use disposable, instant hot packs. Be sure to follow the instructions on the package.
- Apply it in 20-minute intervals.
Psychological/Behavioural
There are also psychological strategies that your student can try to help reduce their pain. These include:
- deep breathing
- relaxation exercises
- distractions (movies or music)
- imagery
What to do when your student with sickle cell disease has a fever
Children with SCD are at greater risk of infections than their peers. This is in part because with SCD, the spleen does not function properly and it is not as good at destroying the cell coating of some bacteria.
Fever in a child with SCD is considered an emergency and requires prompt treatment with antibiotics. Fever is a sign of an infection.
A thermometer should be available at school for assessing the temperature of children if they are unwell. A temperature higher than 38°C under the arm or higher than 38.5°C by mouth requires that the child be seen promptly at an emergency department. Call the child’s caregivers to pick up the child. If they cannot be reached in a short time (perhaps an hour), take the child to the closest emergency department.
Medicines such as acetaminophen and ibuprofen will reduce fever but will not affect the infection that is causing the fever. Using them can lead to a false sense of security or to the fever not being taken seriously. Do not give a student with SCD these medicines to treat a fever.
Fluid requirements and bathroom privileges for students with sickle cell disease
Children with SCD excrete higher volumes of urine compared with their peers because their kidneys cannot concentrate urine. Bathroom privileges are a must whenever the student needs to go. Attempts to hold urine will result in accidents and embarrassment to the student, with the potential for future teasing and bullying.
Correspondingly, when a child produces more urine than usual, they must also increase their fluid intake. This is particularly important in SCD, as dehydration can trigger pain episodes. When a child with SCD is dehydrated, blood cells also become dehydrated and change shape, causing blood vessel blockage and acute pain. A student with SCD should be allowed to have a water bottle at their desk so they have easy access to water. This will reduce the disruption of leaving the classroom for the water fountain.
Sports and extra-curricular activities for students with sickle cell disease
Students with SCD should be encouraged to participate fully to the best of their ability and according to their tolerance level. As a result of low hemoglobin level (anemia), they will tire faster than their peers when doing physical activity. They should be encouraged to try out for school teams and participate in gym, but with more frequent rest periods and increased hydration.
It is a good idea for caregivers and their child with SCD to talk with the physical education teacher about the physical discomforts associated with SCD and any symptoms the student has had in the past with physical activity. The family and the teacher should reach an understanding about expectations.
Special precautions for swimming
Students with SCD can participate in swimming classes. However, they should limit the time in the pool to 30 minutes. After getting out of the water, the student must dry off and change into dry clothing right away. They should not run around in cold, wet swimsuits as their body temperature will fall, potentially resulting in bone pain.
Special precautions for hot weather
When exposed to very hot temperatures, such as during a sporting event in the summer, students with SCD can participate but with frequent rest breaks and increased hydration.
Special precautions for winter activities
Students with SCD should be allowed to participate, but they should be dressed well in layers appropriate for the temperature of the day. Areas of increased loss of body heat, such as fingers, toes, head, and ears should all be well covered. At temperatures less than -5°C, students with SCD should be excused from participating.
Academic performance for students with SCD
Most children with SCD will perform as well as their peers, so expectations for students who have SCD should be similar to those of their peers. Having a chronic illness at times results in reduced self-esteem and lack of confidence. Encouraging the student is essential.
There are several reasons why some students with SCD may have exceptionalities.
Missed school days
Students with SCD may miss school because of:
- scheduled clinic appointments
- hospitalizations to treat infection or the severe bone pain associated with SCD
- painful bone episodes that are less severe and can be treated at home
This means that they have less instructional time. It has been proven that school attendance is directly related to academic performance. A parent could speak with the child’s teacher about setting up a homework buddy program for each student in the class. Each student would have a “buddy” who would collect handouts and notify the absentee student of important future deadlines. Many teachers have websites where they post homework assignments and future dates for both caregivers and students. If these exist, please bring them to the attention of caregivers and students.
Neurological problems
One in five children with SCD have so-called “silent strokes.” These are small strokes in the frontal area of the brain that go undetected unless an MRI is performed. The frontal area of the brain is responsible for executive functioning and this affects a student’s ability to focus, organize, plan, and memorize. As a child who has had a stroke moves to the higher grades they may experience increasing difficulty.
One in 10 children with SCD under the age of 20 years old will have overt strokes. These result in diminished academic performance and various degrees of physical disability. Most overt strokes can be prevented with a chronic transfusion program when children with SCD are identified early in life.
If your student is having difficulty
When a student is identified to be having difficulties academically, neuropsychological testing should be undertaken and appropriate IEP (individual education plan) intervention done on an individual basis. Whenever a teacher is concerned about a student’s health, with the caregivers’ written permission they can seek out the health-care team involved with the student as a resource.
Children with SCD are expected to have a life expectancy well into the sixth and seventh decade, so they should be prepared for the workforce in a manner that is suitable for the adult with SCD.
How teachers can help students with sickle cell disease achieve academically and socially in the classroom
- Learn about SCD and how it has affected your student.
- Provide make-up work for students who have missed days from school due to illness.
- If your student is not performing optimally, suggest a neuropsychological assessment so an IEP can be done to optimize learning.
- Have free and open communication with the student’s caregivers so you can work as a team to optimize performance.
- Dispel any myths or rumours about your student that may be in the classroom, such as reasons for the student’s eyes being yellow or the disorder being contagious.
Special situations where the teacher should call emergency services
If any of the following occurs, call emergency services right away:
- difficulty breathing
- loss of consciousness
- severe headache
- difficulty speaking or slurring of speech
- weakness of limbs
- seizure activity
- fever greater than 39°C (or greater than 38°C and you have not been able to reach the student’s caregivers)
- unexplained sleepiness
- persistent vomiting