What is bronchiolitis?
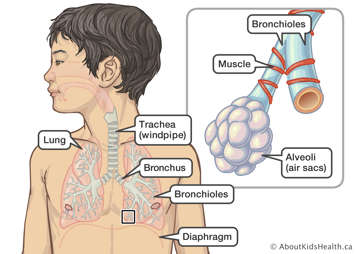
Bronchiolitis is a common infection of the lungs caused by a virus. The infection makes the tiny airways in the lungs swell. These small airways are called bronchioles. The swelling makes the airways narrower, which makes it harder for your child to breathe.
Most cases of bronchiolitis are caused by a virus called respiratory syncytial virus (RSV), although many other viruses can cause it too. Most children will get RSV by the time they are two years old. The infection is most common from November to April, during the RSV season.
Signs and symptoms of bronchiolitis
At first, your child may have a fever, runny nose or cough. Your child will probably cough a lot.
Other signs can include:
- fast, shallow breathing
- high-pitched breathing sounds (wheezing)
- the skin sucking in (indrawing) in the chest below the rib cage, above the collarbone, between the ribs or in the neck; these are called retractions
- flaring of the nostrils
- increased irritability, crankiness or tiredness
- eating or drinking less
- trouble sleeping
At first, your child's cough will probably be dry, short, shallow and weak. After several days, your child may start to bring up a lot of mucus when coughing.
Most children with bronchiolitis are only mildly ill with coughing or wheezing. They do not need any special medical treatment. Bronchiolitis usually lasts about seven to 10 days. In some cases, children can have a cough or mild wheeze that lasts for weeks, even after the virus is gone.
Bronchiolitis can be more severe in some children
Bronchiolitis can be more severe if:
- your baby is younger than three months old
- your child lives in a household with smokers
- your child has asthma or other chronic lung problems
- your child was born prematurely (35 weeks gestation or less)
- your child has certain types of congenital heart disease
- your child has immune system problems
In severe cases, a child with bronchiolitis may need to go to the hospital.
The viruses that cause bronchiolitis spread by coughing, sneezing and touching
The viruses that cause bronchiolitis are spread through tiny droplets that come from an infected person’s nose and mouth when they cough or sneeze. They can also be passed when an infected person touches an object, such as a toy, and another person touches the same object. When children touch their own noses, eyes and mouths, they can infect themselves with the virus. Sharing toys and playing close together increases the spread of infection.
Treating bronchiolitis at home
Most cases of bronchiolitis can be managed at home. Treatment for bronchiolitis usually involves managing the symptoms of the condition.
- Place your child in a partly sitting or upright position. This makes breathing easier.
- Babies should keep breastfeeding or drinking formula as usual.
- If your baby's nose is congested, saline nose drops may help to clear it. This can help your baby feed more easily.
- If your baby is not feeding well, try giving smaller feedings more often. This will help your baby get enough food and liquids.
- Encourage your older child to drink, especially clear fluids such as water or apple juice mixed with water. If your child does not want to drink, try to offer fluids in small amounts more often than usual.
- Do not expose your child to tobacco smoke.
- If your child is allergic to pets or substances in the air, keep them away. These substances irritate the lungs and may make the bronchiolitis worse.
- Do not give cough medicines to children younger than six years old.
- Watch your child for signs of dehydration, such as dry or sunken eyes, dry sticky mouth or less urine than usual.
Treatment in hospital for bronchiolitis
In more severe cases of bronchiolitis, your child may need to be treated in hospital. At the hospital, your child is in a new place that may be a little scary. You can help comfort and calm your child with loving care.
Here is what you can expect while at the hospital.
- Doctors, nurses and other health-care professionals will listen often to your child's chest with a stethoscope. The sounds they hear tell them if your child is breathing well enough.
- Your child will be placed in a partly sitting or upright position to make breathing easier.
- A member of the health-care team may gently suction your child's nostrils.
- Your child may need to breathe extra oxygen. This helps make sure enough oxygen gets into your child's blood.
- If your child is very unwell, their doctor may ask for blood tests or a chest X-ray to be done, or for a tube to be inserted in a vein (intravenous line) or from the nose to the stomach (NG tube). Most children do not need these.
Your child does not need medicines such as antibiotics or antivirals. These medicines will not help. Medicines to treat wheezing usually do not help either. Steroids usually do not help except for in certain situations.
Preventing bronchiolitis
Bronchiolitis is very common and spreads easily, but there are several ways you can reduce your child's risk of catching it.
- Some viruses that cause bronchiolitis, such as RSV, influenza and COVID-19 can be prevented with immunization. Speak to your health-care provider to see if your child is eligible for any of these specific immunizations.
- Good hand washing with soap and warm water is the most effective way to reduce the spread of infection. Wash hands after coming in from outside, after playing with other children's toys and before eating.
- Do not expose your baby to cigarette smoke. Smoking has been associated with increased infection rates. Even second-hand smoke is harmful to your child.
- Try to stay away from infected people or large crowds, especially if your baby is younger than three months old.
- Young children often place toys in their mouths. Clean toys often if they are being shared.
- Teach children to prevent spreading germs by learning to sneeze or cough in their sleeve or elbow. If a tissue is available, children can use it, put the used tissue in the garbage, and then wash their hands.
- If your child goes to daycare or school, tell the caregiver which signs of illness your child has.
- If you can, keep your child at home until breathing is easier.
Children who have trouble breathing must go to the hospital
Take your child to the nearest emergency department if you notice any of the following signs:
- Your child is breathing very fast.
- Your child is having trouble breathing. Look for retractions of the chest or neck, and flaring of the nostrils. These signs are more serious if your child is also wheezing.
- Your child's skin looks blue or paler than usual.
- Your child is not feeding or drinking enough and has become dehydrated. This means your child's body does not have enough fluid to work properly. This can happen when your child is not drinking enough. Your child may be dehydrated if their eyes appear to be dry or sunken or if they are urinating (peeing) less than usual.
- Your child is much more lethargic, or sleepy than usual, and does not want to play.
- Your child is very cranky or fussy and cannot be comforted.
- Your young baby is not able to feed or drink.
Watch this video for more information on spotting signs of breathing trouble in your child.
Your child may show physical changes when their condition is serious or when their condition gets worse. Parents and caregivers can learn how to spot these signs in order to seek help from a health-care provider.