Acne, clinically known as acne vulgaris, is the most common skin disease. It affects 85% of teenagers, some as young as 12, and often continues into adulthood. It is also called "pimples," "zits" or "blemishes".
What causes acne?
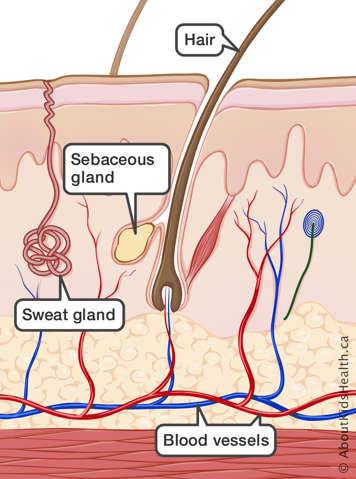
The skin is formed by many layers of tissue, containing hair, glands, muscles, sensory receptors and blood vessels. During puberty, a group of hormones called androgens are released. Androgens allow the sebaceous glands in the skin to produce an oily substance called sebum. Acne is in part caused by this increase in sebum that naturally occurs during puberty.
Normal amounts of sebum keep skin and hair from drying out. However, excess oil can mix with dead skin cells and clog hair follicles (the tunnel that contains a strand of hair) and pores (the opening in the hair follicle on the skin that the hair passes through).
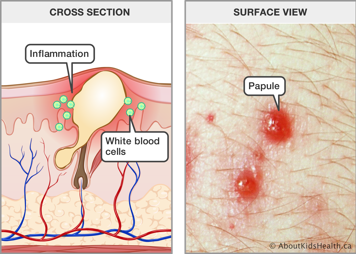
A common type of bacteria that lives on the skin, known as Cutibacterium acnes (C. acnes), sometimes contributes to acne by causing inflammation. The acne signals white blood cells to the area, which damage the tissue and cause an inflammatory response. This causes swelling and infection.
Acne can occur on the face, neck, shoulders, back and chest, where the most sebum is produced.
Acne varies from mild to severe, depending on what kind of blemishes appear. The different types of acne include:
- comedones
- papules
- pustules
- nodules
Comedones
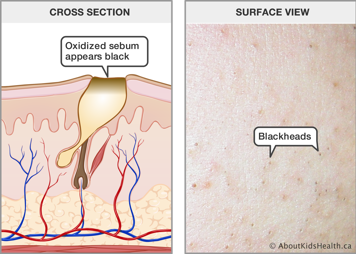
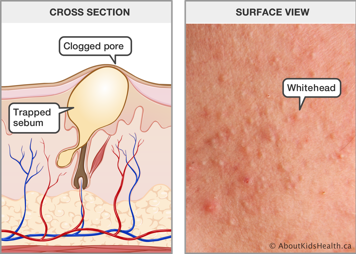
Comedones are pores that are blocked with oil and dead skin cells. They can be open ("blackheads") or closed by the skin ("whiteheads").
A blackhead is generally level with the skin surface and cannot be removed by normal washing of the face.
A whitehead is slightly raised from the skin, but there is no inflammation.
Papules
Papules are red, small, hard bumps that are slightly raised on the skin. In clusters, they can feel like sandpaper to the touch. White blood cells enter the follicle, causing inflammation.
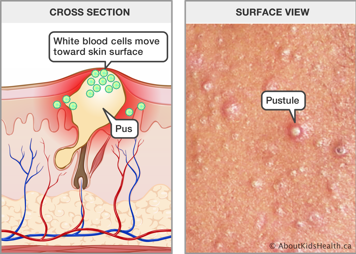
Pustules
When the white blood cells in a papule make it to the surface of the skin, a pustule is formed. Pustules appear as red, inflamed circles with a central, raised bump that is yellowish or white. The bump is filled with pus. Pus is the result of inflammation and contains white blood cells, dead skin cells and bacteria.
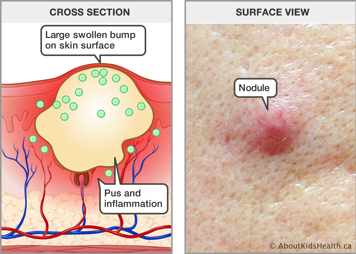
Nodules
When a papule or pustule expands, it can cause more severe inflammation in the surrounding skin. This can lead to nodules, which are deep, red, round bumps that can have a diameter of 6 to 20 millimetres. They are sometimes referred to as cysts.
Nodules are formed by irritated, inflamed hair follicles that have ruptured deep under the skin. They can be throbbing and painful, even without touching.
Psychological impact of acne
Acne can have a profound impact on a person's quality of life, particularly for teenagers. Reactions can range from minimal distress to more significant depression, anxiety and, less commonly, thoughts of suicide or self-harm. For these reasons, treating acne matters.
Treatment of acne
Treatment depends on the severity and type of acne. An effective treatment will help reduce future breakouts and improve the skin's appearance. Keep in mind that up to six weeks of treatment might be necessary to start noticing results. It might take four to six months of treatment to get the full benefit.
In most cases, your child's health-care provider or dermatologist will prescribe topical treatments (applied directly on the skin). Sometimes they may prescribe an oral treatment (taken by mouth).
Cleansing skin
Acne is a process deep within the skin. Washing your face regularly helps remove dead skin cells and excess oil, but it does not play a significant role in the prevention or management of acne. Sometimes, medicated cleansers are used as part of acne treatment. These are cleansers that may help acne through the medication that is applied to the skin through cleansing. These products can often be purchased without a prescription, but your child's health-care provider can provide advice on how to best use these.
If your child has acne, they should avoid scrubbing their face when washing because this may worsen inflammation and irritation. Instead, they should gently wash their face with warm water. They may also use a mild cleansing product if they want.
Topical medications
Topical retinoids
Topical retinoids unplug comedones and improve the process of shedding the old skin cells. They may also help reduce inflammation and the number of new acne lesions that develop. Retinoids can cause very deep but hard-to-see comedones to come to the surface and look more inflamed and prominent.
This is often called "purging". It is the way that retinoids work and most commonly occurs in the first few weeks of using the medication. Sometimes, that makes it seem like the medication is making acne worse, but it is actually part of the treatment and usually settles down within a few weeks.
Some side effects may occur when using a topical retinoid. These include mild irritation, redness, dryness, peeling and sensitivity to sun. People who are pregnant, or those thinking about having a baby, should talk to their health-care provider before using a topical retinoid as they should not be used during pregnancy.
Avoid skin damage, such as waxing or exfoliation (e.g., facials), to the areas being treated with retinoids.
Retinoids are available in many strengths and formulations. Therefore, there is no one better option; your health-care provider will recommend a retinoid that is most appropriate for your child.
Topical anti-inflammatory medications
Topical anti-inflammatory medications are used to reduce inflammation and can reduce bacteria that contribute to inflammation. One option is benzoyl peroxide, which is available over the counter. When benzoyl peroxide touches the skin, oxygen is created. C. acnes cannot survive in the presence of oxygen.
Use caution when applying benzoyl peroxide because it is a potent bleaching agent that can damage fabrics.
In rare cases, benzoyl peroxide can cause an allergic reaction, which could cause significant redness, swelling and/or itching to develop.
Topical androgen blockers
Clascoterone helps block androgens (hormones) from causing the sebaceous glands to secrete excess sebum (oil). The medication can also help reduce inflammation. Unlike many of the other topical medications, this one is used two times per day.
Oral medications (medications taken by mouth)
Oral antibiotics
An oral antibiotic is sometimes used to treat more significant acne, which is mostly made up of inflammatory papules or nodules. Just like topical treatments, oral antibiotics reduce inflammation. Taking antibiotics for a long time can cause problems; for example, it can disrupt the normal bacteria of the gut or cause some bacteria to become resistant to the antibiotic. To reduce these risks, most health-care providers will recommend only using these medications for a short time.
Hormonal therapy
Treating acne with female hormones is an effective treatment option for some female patients. This means taking an oral contraceptive (birth control pill). This type of treatment limits sebum secretion by reducing androgen levels. Other topical and oral treatments can be used along with oral hormonal therapy.
Treating acne using hormones is not for everybody. For more information, talk to your health-care provider.
Oral isotretinoin
Isotretinoin (known as Accutane® in North America; Clarus®, Epuris® and Absorbica® in Canada; and Roaccutane® in Europe) is a chemical compound related to vitamin A. In most cases, isotretinoin is used to treat severe nodular and scarring acne because it:
- reduces sebum secretion
- prevents the formation of comedones
- acts as an anti-inflammatory
- stops C. acnes from multiplying in hair follicles and sebaceous glands
This type of acne treatment must be closely monitored because isotretinoin has a number of side effects. More common side effects include dry skin, lips, nose and eyes. All side effects will begin to disappear when treatment stops.
However, there are more severe side effects. For example, isotretinoin can interfere with the development of a fetus. People who are pregnant or are thinking about having a baby need to talk to their health-care provider about the side effects of isotretinoin. There are also concerns about depression, headaches, joint or muscle aches and pains, and impact on the liver.
Combined treatment
A combined treatment can be an effective way to treat acne. A topical retinoid and an anti-inflammatory cream or gel can be used together. Sometimes, they are combined into one product. Other times, they are used as two different products. For example, a topical anti-inflammatory may be applied in the morning and a topical retinoid may be used at night.
Oral medications are also used in combination with a topical treatment. Most people taking a pill will get added benefit from also using a topical medication.
Your health-care provider will advise you on how and when to use a combined treatment for acne.
Scar prevention
If left untreated, some acne can cause scarring. It is not always easy to predict which acne will cause scarring; it is a complex problem.
Handle acne with care. Manipulating, squeezing and popping increases the likelihood of scarring. The best way to prevent scarring is to actively treat the acne and avoid manipulating the lesions.
When to see a health-care provider for acne
Treatment is not only for those who have severe acne. No matter how little or how much acne your child might have, they can seek treatment for their skin.
