What is cystic fibrosis?
Cystic fibrosis or CF is a disease that mainly affects the lungs and digestive system (or digestive tract). Although CF can be treated and CF patients can usually lead fairly normal lives, there is no cure for CF. Today, half of Canadians with CF live into their 40s and beyond.
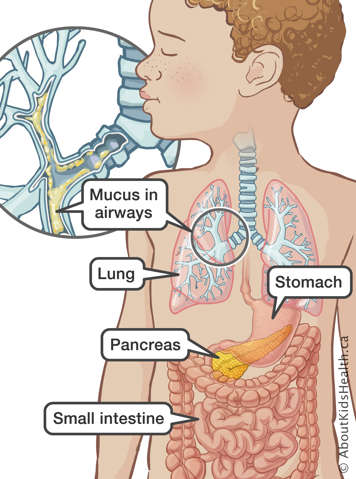
CF affects the lungs
Normal mucus is thin and slippery. It keeps the lungs clean by removing dirt and germs from the lungs' airway tubes. In CF, mucus is sticky and clogs the tubes. This can make breathing difficult. Bacteria can collect in the tubes because the mucus cannot clear as quickly as it should. This leads to cycles of infection and inflammation (swelling in the airway tubes). These infections can damage the lung tissues.
CF may also affect the digestive system
CF may also affect the digestive system, especially the pancreas. The pancreas is an organ just below the stomach that makes enzymes to help digest food in the small intestine. Enzymes help with digestion and break down the food particles small enough to be absorbed. In CF, mucus blocks the ducts (tube-like channels that carry fluid) of the pancreas.
When the ducts from the pancreas to the small intestine are blocked by mucus, the enzymes cannot reach the small intestine. This means food is not properly digested. When this happens, a child with CF does not get enough nutrition from their food. As a result, a child with CF may take replacement enzymes in order to grow normally and may have to eat a bit more food.
Signs and symptoms of cystic fibrosis
In most children, CF mainly affects both the lungs and the digestive system. The symptoms of CF are variable ranging from mild to severe.
Signs and symptoms of CF include:
- trouble breathing
- cough that produces thick mucus
- difficulty gaining weight
- bowel movements that are bulky, frequent and foul-smelling
- skin that tastes salty
- repeated lung infections
- delayed passage of meconium or meconium ileus (a blockage in the small intestine by the newborn's feces)
The symptoms of CF are often confused with other conditions such as asthma, chronic bronchitis, pneumonia or celiac disease because they have similar symptoms as CF.
Cystic fibrosis is a genetic disease
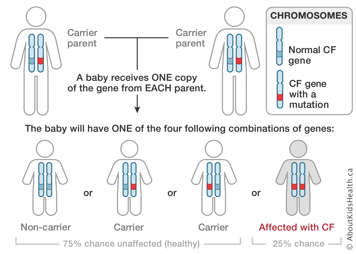
About one in every 3,600 children are born with CF. CF is a genetic disease, meaning it is passed from parents to their children. About one in every 25 Canadians carries the mutated gene that can cause CF. The probability may be lower depending on your ethnic background.
A gene is a section of DNA that gives an instruction to a cell. Most of the time, the instruction is a "recipe" for making a protein.
CF is caused by a mutation in the gene for the CFTR (cystic fibrosis transmembrane conductance regulator) protein. CF is a recessive genetic condition. This means that a person needs to have two copies of the mutated gene to develop CF. People with only one copy of the CF mutation are called "carriers" and do not have symptoms. Most parents do not know they are carriers of the CF gene. To develop CF, a child must inherit two copies of the CF gene, one from each parent.
Two parents with the CF gene may have children with CF, children who are carriers or children who are not. The risk of having a child with CF is the same with each pregnancy.
CF is not contagious. You cannot catch it from someone else.
How cystic fibrosis is diagnosed
In almost all of Canada, babies are diagnosed with CF in the first two weeks of life through the Newborn Screening Program.
- Genetic tests are used to diagnosis CF. Genetic tests can diagnose CF before a child is born.
- Shortly after a baby is born, the doctor may take a small sample of blood from the baby as part of the newborn screening program. Testing starts by looking for an enzyme called IRT. If the level of IRT is high, the doctor will perform a DNA test looking for the most common CF mutations. If the screen is positive, the doctor will refer your child to a specialist centre for confirmation and follow-up.
- Doctors usually order a sweat test if they suspect CF. This is a simple test that measures the amount of salt in the sweat. It will not hurt your child. Heat or medicine is applied to a local (small) area of the skin. If the sweat contains more salt than usual, this may mean your child has CF.
- Doctors may perform a test to check for enzymes in the intestine.
How cystic fibrosis is treated
There is no cure for CF. With appropriate treatment and regular follow-up, most children with CF can live fairly normal lives up to at least their 40s.
CF treatment is tailored to your child's needs. It also depends upon the stage of the disease and which organs are affected.
Treating the lungs
A lot of CF treatments focus on the lungs. The treatments work to loosen and thin the mucus that clogs the airways. Chest X-rays may be taken to see if there are any changes in the lungs.
Treatments followed at home may include:
- Physiotherapy is done by tapping or "clapping" on the chest in different positions twice a day for babies and young children.
- PEP (positive expiratory pressure) mask therapy is taught to older children and adults with CF to help clear their lungs.
- Other forms of chest physiotherapy to help loosen the mucus that clogs the lungs can also be taught by the clinic physiotherapist.
- Oral (through the mouth), inhaled (breathing) or intravenous (IV or using a needle) antibiotics are often used when someone with CF has a lung infection.
- Exercise.
- Medications to help open the airways and thin mucus are inhaled using a puffer or a small compressor machine with a nebulizer, which makes the medication easy to inhale through a mask or a mouthpiece.
To avoid infection, children with CF should also:
- Avoid contact with people with a cold or illness
- Avoid contact with other people with CF
- Have their usual immunizations (shots)
In some cases, when treatments can no longer maintain a person's health or organ function, the person may require a lung transplant.
Treatments for the digestive tract include:
- taking pancreatic enzymes with meals to help digestion
- taking supplements and special CF vitamins to promote good nutrition
- eating a special diet with increased calories and fat
- adding salt to the diet to replace the excess amounts lost by sweating
Activity
Children with CF are encouraged to play games and sports. Ask your child's doctor how much activity they can do. Sports such as running and swimming are often helpful because they help clear the lungs of mucus.
Children with CF lose a lot of salt during exercise and hot weather, more than people without CF do. It is important to make sure your child replaces fluids and salt by drinking enough and eating enough salt.
