What are undescended testicles?
Testicles are male reproductive organs that form in the fetus during pregnancy. They move from the body through a tube in the groin called the inguinal canal before descending into the scrotum before birth. The scrotum is the sac of skin hanging behind the penis.
An undescended testicle means that the testicle has not lowered into the scrotum before birth. This is called cryptorchidism and can happen to one or both testicles.
The condition is common among premature babies. All babies with male anatomy are examined after birth to make sure their testicles have descended.
You can feel for your child's testicles while changing diapers or while bathing. If the testicle does not descend on its own by three or four months, your child should see their health-care provider. They may need surgery.
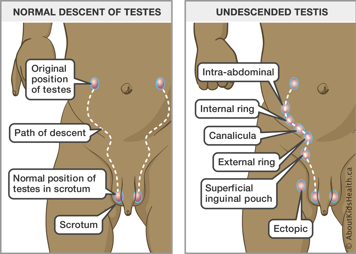
Types of undescended testicles
- An inguinal testicle: the testicle is felt in the inguinal canal.
- Non-palpable testicle: the testicle cannot be felt or “palpated” in the scrotum or in the inguinal canal.
- A retractile testicle: a testicle that can be felt in the inguinal canal (groin area) and brought down to the level of the scrotum; however, it moves back up into the inguinal canal when released.
Risk factors
Undescended testicles happen because of problems during fetal development. Risk factors that may increase the likelihood of problems during fetal development include:
- premature birth
- family history of undescended testicles
- low birth weight.
Diagnosis
Undescended testicles are diagnosed by physical exam by a health-care provider. An ultrasound of the testicles is not routinely required to diagnose undescended testicles but may be requested at the discretion of your child’s health-care team. They may also request additional studies if both testicles are undescended.
How a health-care provider can help your child with an undescended testicle
If the testicle has not lowered into the scrotum, your child’s health-care provider will try to manually move the testicle into the scrotum. If this does not work, the health-care provider may refer you to a urologist—a health-care provider that specializes in the urinary tract and the male reproductive system.
If the testicle has not descended on its own by three or four months of age, your child may need surgery (orchidopexy).
What is orchidopexy?
Orchidopexy is an operation to lower the testicles into the scrotum. Your child may need to have this operation on one or both testicles. The orchiopexy surgery may need to be done in stages, involving one to two operations. Depending on the assessment by your child’s health-care provider, the surgeon may use an “open” approach (with cuts at the level of the scrotum) or a laparoscopic approach (with smaller incisions in the abdomen).
For more information on how to prepare for and what to expect on the day of your child’s procedure, see the Coming for surgery learning hub.
Complications of undescended testicles
Testicles need cool body temperature in the scrotum area to make sperm. An undescended testicle may be too warm to produce healthy sperm. This increases the risk of fertility problems later in life.
An undescended testicle also cannot be easily felt or “palpated”. As children get older, this means they may be unable to self-examine for testicular masses or cancer.
Caring for your child at home after the operation
Pain relief
Your child will feel soreness in the groin for the first few days after the operation. They will likely need to take acetaminophen or ibuprofen for pain on a schedule for the first few days and then only as needed. Please give medications to your child as instructed by their health-care team.
In younger children, look for these signs of pain:
- Irritability or difficulty sleeping
- Increased sweating
- Not behaving like their usual self
Surgical site care
- The stitches from the procedure are absorbable and do not need to be removed.
- Surgical glue will be used to close the incision sites. This looks like a clear to white seal. The glue will start to flake off after a few days. Do not pick at the glue to remove it. It will fall off on its own.
- It is normal to have bruising and discolouration with some swelling after surgery. This should gradually improve overtime. If the swelling is unchanged and/or painful for your child, return to the hospital for re-assessment.
Diet
The evening after surgery, your child can slowly advance their diet to clear fluids (e.g., water), then full fluids (e.g, juices, smoothies, soups) before eating as usual. If your child is still breastfeeding or bottle feeding, you should offer these to your child on their usual schedule but start with small volumes and increase as tolerated (ensuring that they are not vomiting). They may feel some nausea due to the anesthetic. By the first day after surgery, your child should be able to eat as usual.
Peeing and bowel movements
Your child should continue to pee every few hours and have bowel movements once daily at minimum. If your child is in a diaper, ensure the surgical site is cleaned well with soap/water and gently patted dry after every bowel movement.
Activity
Your child should avoid certain activities for a few weeks after surgery. These activities include:
- strenuous activities that require a significant amount of physical effort
- contact sports that may result in trauma to the area (e.g., football or hockey)
- riding a bicycle
- use of hot tubs or public pools.
Follow-up
Your child will be scheduled for routine assessment approximately three months after orchiopexy surgery. This allows enough time for the swelling and discoloration of the surgical site to resolve.
While you are waiting for your appointment, routinely check to see that your child’s testicles are down in the scrotum on both sides. There is a risk of the testes twisting or rising back up even after orchiopexy surgery is completed.
When to seek medical assistance
If you think a diagnosis of undescended testicles has been missed, see your child’s primary health-care provider. See a health-care provider if you have any concerns about the area around your child's groin.
Warning signs after surgery
Contact your child’s health-care team if your child has signs of infection such as:
- increased pain at the incision line
- redness at the incision line
- swelling or puffiness at the incision line
- any non-clear drainage from the incision (e.g., green/yellow pus, fresh red blood)
- a fever higher than 38°C
- vomiting or not tolerating any food or fluids by mouth
- abdominal pain that is not relieved by acetaminophen or ibuprofen
- paleness, lethargy or feeling unwell.
Bring your child to the Emergency Department immediately if:
- they have severe pain or swelling of the testicle
- the testicle is no longer visible in the scrotum
- the pain is unmanaged by prescribed medications
- they have difficulty urinating or they’re unable to pee for more than six to eight hours.
