What is an anorectal malformation?
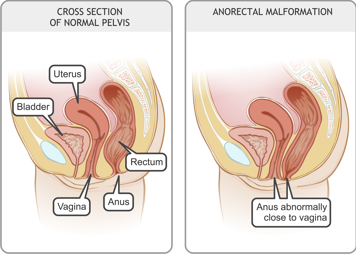
An anorectal malformation is a birth defect that causes the anus not to develop properly. It occurs in one in every 4,000 babies.
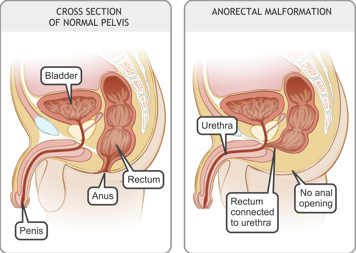
Some children are born with an anal opening that is too small, some have an anal opening that is in the wrong place and some have no anal opening at all. This can happen if the end of the intestine does not separate properly from your child's urinary system (in boys) or their vagina (in girls) while they are still in the womb.
A child who is born with an anorectal malformation might also have problems in other areas of their body. Your doctor will do tests to check for these problems soon after your child is diagnosed.
How anorectal malformation is repaired
Your child may need surgery (an operation) to repair the malformation.
If the opening is too small
If the anal opening is in the right place but is simply too small, the doctor may only need to use a special dilator to slowly stretch it to make it the right size.
If the opening is in the wrong place
If the opening is in the wrong place, the surgeon may perform a surgery called anoplasty (see below) to put the anus in the right place.
If there is no opening or if the opening is far away from where it should be
If your child's anal opening is very far from where it should be, or if there is no opening at all, the doctor will need to create an ostomy for your child within 24 to 48 hours of birth.
When your child is a little older, they will normally have a posterior sagittal anorectoplasty (PSARP), or Peña procedure, to create the anus in the right place. This is explained below.
During the surgery
If your child needs an ostomy, anoplasty or anorectoplasty, they will have a special "sleep medicine" called a general anaesthetic. This means that your child goes to sleep and does not feel any pain during the operation.
Ostomy
An ostomy is an opening created from the inside of the body to the outside, on the tummy (abdomen). Stool passes through it and is collected in a pouch that is attached to your child's abdomen. In most cases, this ostomy is only temporary.
Once your child has an ostomy, they will be like any other baby except that they will stool into the pouch. Before you leave the hospital, your health-care team will teach you how to care for your child's ostomy and when to call the doctor.
Anoplasty
This usually involves gently stretching your child's anal opening over several months and then performing surgery to move the anus when your child is older, before they start solid food.
Posterior sagittal anorectoplasty
A posterior sagittal anorectoplasty usually involves disconnecting the end of the intestine from the urinary system (for boys) or from the vagina or beside the vagina (for girls). An opening is then created to allow stool to come out of the intestine at the right place.
If the connection was very high, the surgeon will sometimes do some of the surgery through your child's abdomen. This is usually done with a laparoscope (a small camera inserted through your child's belly button) and requires only tiny incisions (surgical cuts).
After the surgery
Your child can go home when:
- their heart rate, breathing, blood pressure and temperature are normal
- they can eat without vomiting (throwing up)
- they are comfortable taking oral pain medicine (medicine taken by mouth)
- the stoma is working well
- your child's doctors and nurses have finished teaching you how to care for your child after surgery.
Follow-ups with the surgeon
Your child will have their first follow-up with the surgeon two to three weeks after the anoplasty or anorectoplasty. It is very important that you attend this follow-up appointment when it is scheduled.
The surgeon will check your child and make sure that the stitches at the anus are healing properly. They will do this either by inserting their finger or using an instrument called a Hegar dilator. You may need to buy the Hegar dilator (it is not expensive).
Dilations after surgery
The surgeon may bring your child back for rectal calibration (gentle stretching of the new anus) with a finger or Hegar dilator or will teach you how to do it at home. Your child may need these dilations for several months after surgery. It is very important for your child's care that you meet with your surgeon and follow their instructions. If the anus does not heal properly, your child may need more surgery.
When your child can start stooling normally
When your surgeon is sure that your child has fully healed from the anoplasty or anorectoplasty, they will perform another operation to close your child's ostomy.
Your child will then start stooling from their anus and have many stools a day. As your child's bottom has never had stool on it before, they will be prone to diaper rash. The nurse will teach you how to apply special ointments or creams to your child's bottom before you bring your baby home from hospital.
Taking care of your child at home
- Give your child a bath every day.
- After the anoplasty or anorectoplasty you will see stitches around your child's new anus. Place an antibiotic cream on top of the stitches (do not rub it in) three times a day until you see the doctor in follow up.
- Do not put anything into your child's bottom (for example a temperature probe) until your doctor tells you it is okay to do so.
- Bring your child for follow-up appointments and follow any special care instructions.
- To prevent diaper rash, apply ointments or creams to your child's bottom when they first start stooling from their anus.
Long-term effects of anorectal malformation
Some of the muscles and nerves around your child's anus may not have formed properly. This means that your child may have lifelong problems with bowel control or
constipation. For example, your child's toilet training for stool may take longer than it does for another child or they may not be able to toilet train at all.
It is difficult to know for sure what problems, if any, your child will have until they reach the age of toilet training. Because of this, your child will need to be followed closely by their surgeon until toilet training is finished, and on into later childhood and adolescence.
Your surgeon and the surgical team will work closely with you and your child to make a bowel management plan so that your child will be able to wear underwear to school when the time comes. The plan might include having a special diet, using special medications or having enemas.
When to call the surgery team
Call your surgeon's office if:
- your child has a fever of 38°C (100°F) or higher
- your child is in pain
- your child is vomiting (throwing up)
- your child has more frequent or less frequent bowel movements than they normally have
- your child has a swollen belly or serious diaper rash
- there is redness or swelling around the incisions
- there is no stool from the stoma
- the stoma is retracted (pulled back inside the skin) or prolapsed (coming out too far from the skin)
- the stoma is bleeding.
You can also call if you have any other concerns about your child.
Sources
American Pediatric Surgical Nurses Association. Posterior Sagital Anorectoplasty — PSARP (Pena procedure) Teaching Sheet.