There are several complications of JIA which may or may not affect your child, depending on the type of JIA they have, how severe it is, and how well it is managed. Complications can affect various parts of the body from bones and joints to the muscles and eyes.
Unpredictable flares in JIA
Sometimes, young people with JIA can go for months or even years without their disease bothering them, but then it comes back. This is called a flare-up or flare. Most young people have ups and downs in their symptoms for many years, depending on what type of JIA they have. It is important to remember that flare-ups just happen and can’t be prevented. Usually, the cause of the flare is unknown. It can be upsetting to see such changes when it seemed like the JIA had improved or disappeared. Do not give up hope. There are many excellent treatments available to help get the inflammation back under control.
Growth problems in JIA
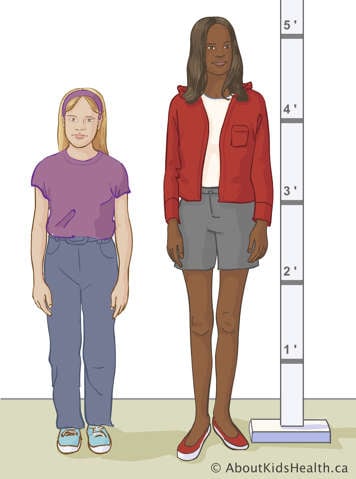
Young people who are still growing have growth plates at the end of their bones. These growth plates fuse or close when they have reached their adult height. The inflammation of JIA can affect how the body grows. Inflammation causes an increase in blood flow to the growth plates, which leads to more rapid growth of the bones in the affected joints. Therefore, the side affected by arthritis may be larger or longer than the unaffected side.
However, in some cases, the inflammation can cause the growth plate to fuse or close earlier than it was supposed to. This can cause the affected side to be smaller or shorter than the unaffected side. Jaw inflammation can result in a smaller or misshaped chin. Knee inflammation can lead to one leg being longer than the other. Occasionally, if the JIA is severe, overall growth (height) might be slow. Your child's growth will usually improve once the inflammation settles.
Some of the medications your child takes to manage JIA, such as corticosteroids, may also slow their growth. Keeping JIA in good control with medications is the best way to avoid these types of growth problems. The health-care team will pay careful attention to your child's growth.
Joint contractures in JIA
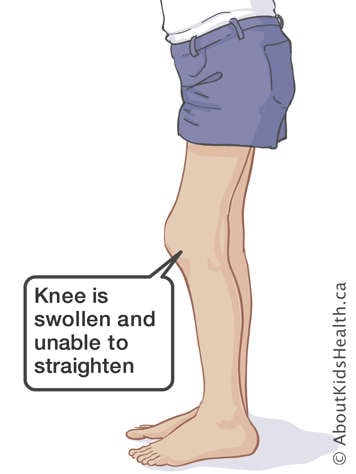
Inflammation causes pressure and sometimes pain in and around the joint. Sometimes, children and teens with JIA will keep the inflamed joint in the most comfortable position, which is usually bent. If a joint stays bent for too long, both the muscles and the structures that attach muscles to bones, called tendons, will shorten and not grow properly. As a result, the joint becomes stuck in a bent position. This is called a joint contracture.
In children and teens, unlike adults, cartilage and bone can still grow. This allows for healing and repair of joint damage. Joint tightness can be reduced with regular stretching exercises and splinting. A splint is a brace that helps to keep a joint (like your knee or your wrist) in one position.
Sometimes an
injection of medicine into the joint is very helpful. It can rapidly decrease the inflammation in the joint so that your child can do the stretching exercises more effectively.
Muscle weakness and muscle loss in JIA
Muscle weakness and muscle loss around an inflamed joint are common in people with JIA. When a joint is swollen, stiff, and painful to move, it is natural for your child to want to reduce their activities. However, doing this can make their muscles weaker. When muscles are not used regularly, they will become smaller.
Exercising helps prevent muscle weakness or even muscle loss. Using a brace or splint might not help, because they prevent the muscles from working properly. Talk to your child's doctor or physiotherapist about how to improve muscle strength safely.
Osteoporosis in JIA
Osteoporosis is when the bones become thin and weak. Bones with osteoporosis are easy to fracture. Osteoporosis can develop in young people with JIA for many reasons. These include not staying active and not getting enough calcium, both of which are needed to help make bones strong and healthy. Taking certain medications like corticosteroids for a long time may also lead to osteoporosis. Prolonged joint inflammation or arthritis can also lead to osteoporosis.
You can help prevent osteoporosis by staying active. Your medical team may also ask you to take calcium and vitamin D supplements. You might need special bone density tests once in a while to check for osteoporosis. You will learn more about this in the Diagnosis section.
Eye problems and JIA
In addition to joint problems, JIA may cause problems with your eyes including uveitis, glaucoma, or cataracts. All young people with JIA should get their eyes checked regularly by an ophthalmologist or optometrist. An ophthalmologist is a medical doctor with special training in eye care and treatment. An optometrist is a health care professional who can diagnose eye problems. Your rheumatology team will let you know how often you need to see your eye doctor.
For more detailed information about uveitis, glaucoma, and cataracts, see the next page in this session, entitled "Eye problems."
