What is analgesia?
Analgesia is another name for pain relief. While your child recovers from surgery in the hospital, they may be given opioid medication such as morphine, hydromorphone or fentanyl to relieve severe, acute (short-term) pain. These drugs are usually used for a limited time.

How is the medication controlled?
The medication can be controlled through:
- patient-controlled analgesia (PCA)
- nurse-controlled analgesia (NCA)
Patient-controlled analgesia
With patient-controlled analgesia (PCA), the patient (your child) decides when they need medication to relieve their pain.
Nurse-controlled analgesia
With nurse-controlled analgesia (NCA), a nurse decides when your child receives pain relief. NCA is used when a patient needs to access pain medication quickly or frequently, but they cannot deliver it themselves, for instance because of their age, physical ability or developmental stage.
How do PCA and NCA work?
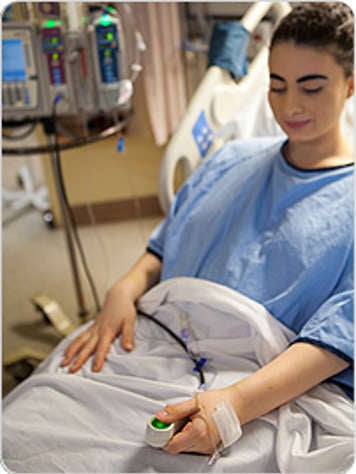
For both PCA and NCA, medication is delivered through a special pump that is connected to an intravenous line (IV). This is a small tube put into a vein in your child’s arm or leg to give medicine or fluids. When a button attached to the pump is pressed, your child receives a small dose of medication through the IV line.
Usually your child will get pain relief right away, but other times it may take a few minutes for the medication to take effect.
The pump provides opioid medication in “as needed” doses, but it can also be programmed to provide a constant infusion, or flow, of opioid medication. You can ask your child’s nurse or a healthcare provider from your hospital’s pain service how your child’s pump is set up.
How safe are PCA and NCA?
When used properly, PCA and NCA therapy are very safe forms of pain relief. Two safety features built into the pump prevent your child from ever receiving too much medication.
- A lock-out period gives the medication time to work and prevents it from being delivered even if the button is pressed repeatedly.
- A maximum dose setting (decided by your child’s health-care team) limits the total amount of medication your child receives.
How do I make sure my child uses PCA or NCA properly?
Patient-controlled analgesia
- Only the patient (your child) decides when they need pain relief and pushes the button on the pump to deliver the medication. This is very important for safety reasons.
- Your child should always be able to easily reach the button on their pump.
- Your child can press the button before a painful activity or procedure, such as coughing, walking, physical therapy or dressing changes.
- If, after one button push, the pain is not relieved in a few minutes, your child can press the button again.
- If your child’s pain is not relieved after a few pushes, you or your child should let the nurse know.
Nurse-controlled analgesia
- Only your child’s nurse pushes the button on the pump. This allows the nurse to monitor your child closely.
How effective are PCA and NCA?
PCA and NCA offer fast and effective pain relief when they are used as instructed and for the exact pain for which they were prescribed.
Remember that they may not be helpful for other pains. For instance, the opioid medication in a PCA or NCA pump might not ease pain from a non-surgical headache or from stomach pain due to nausea or gas.
Other options for pain relief

If your child experiences new or different pains, they may be prescribed other medications such as acetaminophen, ketorolac (an intravenous anti-inflammatory medication) or ibuprofen. If used correctly, these medications may help reduce the amount of opioid medication that your child needs.
Does the PCA or NCA medication have side effects?
The side effects of opioid medication include:
- nausea and vomiting
- constipation
- itching
- difficulty passing urine
- drowsiness or slowed breathing.
Nausea and vomiting
Opioids are most likely to cause nausea and vomiting. Your child’s healthcare team may prescribe other medications, such as dimenhydrinate (Gravol) or ondansetron (Zofran), to help with this.
Constipation
Constipation can be relieved with some medications. Drinking plenty of fluids and going for walks or doing some light exercise can also help.
Itching
Itching (especially around the face and chest) is a less common side effect of opioids. It may be managed with other medications or by changing the type of opioid medication in the PCA or NCA.
Difficulty passing urine
Less often, opioids can cause urinary retention (difficulty passing urine). This is sometimes treated by changing the dose or type of opioid medication. In rare cases, a child may need a urinary catheter to help empty the bladder.
Drowsiness or slow breathing
Sometimes, higher doses of opioids cause drowsiness or slow down breathing. Sleep is important for healing, but if it is difficult for your child to stay awake, especially right after using the PCA or NCA button, it is important to tell your child’s nurse.
How will my child be monitored for side effects?
Nurses closely monitor all patients who use PCA or NCA. Because the side effects of this medication include drowsiness and slowed breathing, your child’s pulse (heart beat) and oxygen saturation (the amount of oxygen in their blood) will be monitored constantly.
Your child’s nurse will also monitor for other medication side effects and check if the medication is working properly to reduce pain.
What can I do to help ease my child’s pain safely?
Patients and family members play a very important role in pain management.
Follow instructions
It is very important that you follow all medication instructions from your child’s health-care team. Never press your child’s PCA or NCA button.
Patient-controlled analgesia
For safety reasons, it is important that only your child pushes the PCA button. A patient who is asleep or drowsy should not receive any medication until they are alert enough to use the button on their own.
Nurse-controlled analgesia
If your child uses NCA, it is important that only nurses press the button so they can monitor the effects of the medication on your child.
Communicate with your child’s health-care team
Tell your child’s nurse or the hospital’s pain service if your child’s pain is not being eased by the medication or if they are experiencing side effects.
Similarly, tell your child’s nurse if your child has any new or different pains so that your child can receive other treatments.
Remind your child to use pain relief
If your child is using PCA, remind them to push the button for pain relief when they need it.
Use medications as part of the 3 P's of pain management
Pain is often treated using the “3 P's of pain management”:
- pharmacological strategies (medications)
- physical strategies
- psychological strategies.
Besides taking medications as instructed, your child can use physical strategies such as heat or cold packs, stretching, exercises, repositioning or massage. You can also encourage your child to manage their pain through psychological strategies such as distraction, playing games, deep breathing, meditation and guided imagery.
Together, the 3 P's can reduce your child’s pain and the impact of pain on your child’s time in hospital. Talk to your health-care team about how to build these strategies into your child’s pain management plan.
If your child is involved in their treatment, share with them the handout Five Questions to Ask About My Medicine. It will help them be better prepared when meeting with their health-care team.
How long will my child need to use PCA or NCA?
PCA and NCA are intended for short-term use. Your child will stop using them when:
- their pain has been relieved or
- they can take medication by mouth or through a feeding tube.
Although it is not very common, PCA and NCA can sometimes be used for longer-term pain relief. Talk to your child's health-care team if you have questions about their specific therapy.
At SickKids
The Acute Pain Service (APS) is a team of pain specialists that looks after all patients with PCA and NCA and provides care to many other hospital patients who have pain.
The service includes anaesthesiologists (doctors who provide sleep medicine and control pain for surgery, procedures and certain illnesses), advanced practice nurses and a psychiatrist. They work closely with other members of your child’s healthcare team to make sure your child’s pain is managed effectively.
If you are using PCA or NCA, you can expect a daily visit from the APS. The team also has an anaesthesiologist on-call overnight to deal with any urgent concerns.