What is a chest tube or pleural drain?
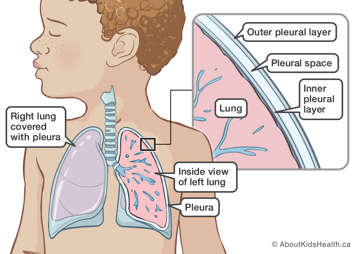
A chest tube (pleural drain) is a soft flexible tube placed into the space around the lung, called the pleural space. Chest tubes drain fluid or air that may affect your child's breathing. They may be inserted by a surgeon as part of an operation or at the bedside by a health-care provider in some areas of the hospital.
Chest tubes are inserted by an interventional radiologist using ultrasound and X-ray.
Why is a chest tube needed?
After an operation or serious injury, or as a result of disease, the pleural space can fill up with air, blood or fluid. The air or fluid in the pleural space stops the lungs from inflating completely when your child breathes in. As the amount of fluid or air in the pleural space increases, it becomes more and more difficult for your child to breathe. The air or fluid needs to be drained away from the pleural space. This is done by inserting a chest tube.
Risks of chest tube insertion
Chest tube insertion is usually considered a low-risk procedure. The risk may increase depending on your child's condition, age and health.
The risks of a chest tube insertion include:
- pain or discomfort
- leakage of air back into the pleural space
- infection
- worsening breathing problems
Giving consent before the procedure
Before the procedure, the interventional radiologist will go over how and why the procedure is done, as well as the potential benefits and risks. They will also discuss what will be done to reduce these risks and will help you weigh the benefits against the risks. It is important that you understand all the potential risks and benefits of the chest tube insertion and that all your questions are answered. If you agree to the procedure, you can give consent for treatment by signing the consent form. A parent or legal guardian must sign the consent form for young children. The procedure will not be done unless you give your consent.
How to prepare your child for the procedure
Before any treatment, it is important to talk to your child about what will happen. When talking to your child, use words they can understand. Let your child know that medicines will be given to make them feel comfortable during the procedure.
Children feel less anxious and scared when they know what to expect. Children also feel less worried when they see their parents are calm and supportive.
Food, drink, and medicines before the procedure
- Your child's stomach must be empty before sedation or general anesthetic.
- If your child has special needs during fasting, talk to their health-care provider to make a plan.
- Your child can take their regular morning medicine with a sip of water two hours before the procedure.
- Medicines such as acetylsalicylic acid (ASA), naproxen or ibuprofen, warfarin, or enoxaparin may increase the risk of bleeding. Do not give these to your child before the procedure unless they have been cleared first by their health-care provider and the interventional radiologist.
Your child will have medicine for pain
It is important that your child is as comfortable as possible for the procedure. They may be given local anesthesia, sedation or general anesthesia. The type of medicine that your child will have for the procedure will depend on your child's age and condition.
During the chest tube insertion, you will be asked to wait in the surgical waiting room.
How a chest tube is inserted
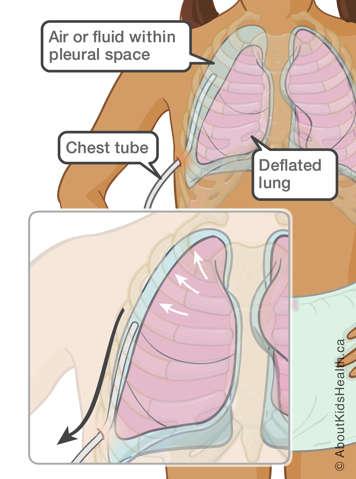
A small incision (cut) is made between the ribs. The interventional radiologist uses ultrasound and a type of X-ray called fluoroscopy to see the tube as it is tunneled under the skin into the pleural space.
The chest tube is secured with a dressing and a device to protect it and keep it securely in place.
The tube is connected to a collection container. The collection container needs to be placed below the level of the bed so the air or fluid can drain out. If your child needs suction, then their chest tube may be connected to suction coming from the wall in their room. You may notice a bubbling sound from the suction.
If your child does not need suction for their chest tube, then it will only be connected to a collection container that drains using gravity.
The tube will need to stay in place until there is little left to drain from the pleural space. Usually, your child will need to stay in hospital until the chest tube is removed and the underlying problem is resolved. This varies depending on your child's condition.
After the chest tube insertion
Once the chest tube insertion is complete, your child will be moved to the recovery area. The interventional radiologist will come and talk to you about the details of the procedure. As soon as your child starts to wake up a nurse will come get you.
The interventional radiologist will come to see your child after they have settled in the recovery area to ensure the chest tube is working properly.
Some children feel local pain or discomfort after the chest tube is placed. The tube is thin, and pain can usually be controlled by pain medicines. Your child will be closely monitored and given pain medicine as needed. After a day, most children feel no pain with the tube.
Taking out the chest tube
Your child will not need anesthetic when the chest tube is taken out. The chest tube is usually removed at the bedside, and a sealed dressing is placed over the chest tube site. Your child will not need any stitches.
The dressing over the chest tube site will stay in place for a few days (at least 48 hours). Your child's health-care provider will tell you when the dressing can be taken off. You will receive instructions on how to take care of the site.
Going home
The length of your child’s hospital stay will depend on their overall health. In most cases, children go home only after the chest tube is removed. Their health-care provider will let you know when they are well enough to go home.
At SickKids
The interventional radiologists work in the Department of Diagnostic Imaging – Division of Image Guided Therapy (IGT). For more information on chest tube insertion using image guidance, please call the IGT clinic at (416) 813-7654 ext. 202407. Speak to the IGT nurse practitioner during working hours or leave a message with the nurse practitioner.
For more information on preparing your child for their procedure see Coming for surgery.