What is hereditary spherocytosis?
Hereditary spherocytosis (HS) is a genetic blood disorder of the red blood cells. Red blood cells contain hemoglobin, which is the molecule that carries oxygen from the lungs to the rest of the body.
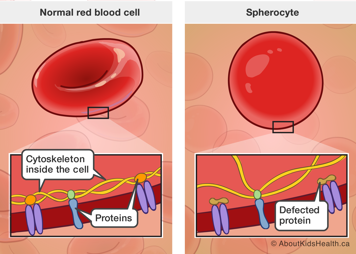
Red blood cells are usually shaped like a disk, with a depressed centre, like a donut without a hole. In HS, most red blood cells are circular and shaped like spheres. These are called spherocytes.
HS is the most common form of inherited hemolytic anemia. “Hemolytic” refers to hemolysis, which is the breakdown of the red blood cells. Anemia is a lack of either hemoglobin or red blood cells in the body.
Signs and symptoms of hereditary spherocytosis
Common signs and symptoms of HS include:
- symptoms of anemia including pale skin (pallor) compared to your child’s normal colour, low energy (fatigue), irritability
- signs of jaundice including yellowing of the skin and the whites of the eyes
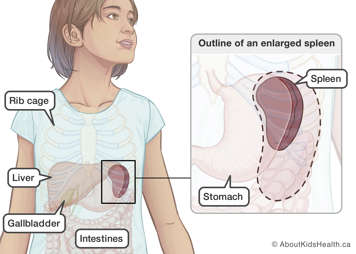
- enlarged spleen (also known as splenomegaly)
The severity of symptoms varies from one child to another but is typically the same among affected family members. However, this may vary in some cases.
HS can be categorized as mild, moderate or severe.
- About 20-30% of people with HS have a mild form.
- The majority (60-80%) of people with HS have a moderate form.
- A small number of people with HS (10-20%) have a severe form of HS.
The severity of the disease depends on the degree of anemia. This is based on your child’s:
- baseline (typical) hemoglobin level
- reticulocyte count (immature red blood cells)
- bilirubin level
- spleen size (if the spleen is enlarged i.e. splenomegaly)
Causes of hereditary spherocytosis
Spherocytes are round because they have a defect in the internal framework, called the cytoskeleton. Every cell in the body has a cytoskeleton, which is made of specialized proteins. These proteins assemble neatly in a sturdy but flexible network that gives each cell their particular shape and elasticity. Due to the defect in HS, the cells become more rigid and less flexible.
In HS, there is a defect in one or more of the five proteins of the cytoskeleton. This defect impacts only the red blood cells. Spherocytes are not as flexible as normal red blood cells and cannot move through the spleen as easily. This causes the spherocytes to be trapped and destroyed in the spleen. Although it is part of the spleen’s job to filter and destroy red blood cells, in HS red blood cells become trapped faster than the spleen can destroy them. This causes the spleen to grow bigger (enlarged) over time. Doctors may refer to an enlarged spleen as splenomegaly.
As a result of this constant breakdown (hemolysis), the contents of red blood cells are released. This creates the following health issues:
- Anemia (low hemoglobin)
- Jaundice; when hemoglobin is broken down, it forms bilirubin that can cause the skin and whites of the eyes to appear yellow
- Gallstones can develop because of increased red blood cell turn over
Inheritance
In most cases, HS is an inherited genetic condition, which means that the genes involved in HS are typically passed down from one or both parents to their children.
For more information on how HS is inherited, please see Hereditary spherocytosis: Genetics.
Diagnosis of hereditary spherocytosis
HS can be diagnosed at any age from infancy or childhood to adulthood. Babies and children with HS are usually diagnosed because they appear jaundiced and/or anemic.
Blood tests
To diagnose HS, your child will need the following blood tests:
- Complete blood count (CBC): a CBC measures the number of different cells in the blood and measures the number of red blood cells to test for anemia.
- Reticulocyte count: indicates how quickly young red blood cells, called reticulocytes, are being produced and released from the bone marrow.
- Blood smear: a blood sample is examined under a microscope to see the size and shape of individual blood cells.
The CBC may show a decrease in the hemoglobin and an increased reticulocyte count. People with HS have an increased number of reticulocytes because the bone marrow is producing more red blood cells to compensate for the hemolysis. The blood smear may show spherocytes.
A blood smear is usually enough to diagnose HS, however additional blood tests may be needed.
Abdominal ultrasound
Your child’s doctor may order an abdominal ultrasound once your child reaches school age (or earlier, if necessary). The abdominal ultrasound will help measure the size of the spleen and show if there are gallstones in the gallbladder.
Treatment of hereditary spherocytosis
HS is a lifelong condition. Treatment usually involves treating and managing the symptoms of HS.
Phototherapy
Jaundice can be a problem in the newborn period if the bilirubin levels are too high and may require treatment, such as phototherapy. Phototherapy involves exposing the skin to a special blue light that changes bilirubin to a form that can be passed out of the body more easily.
Blood transfusion
In some cases, a blood transfusion is required for severe anemia. This is most common in the first year of life but may be ongoing if the anemia is severe. Most children with HS do not need blood transfusions on a regular basis.
Your child’s doctor will decide if a blood transfusion is needed and will discuss the risks and benefits with you.
Splenectomy
Some children with HS may benefit from having a portion (partial splenectomy), or all (full splenectomy), of their spleen removed. This surgery is called a splenectomy.
The spleen plays an important role in protecting the body from certain bacterial infections, thus it is best to delay a total splenectomy as long as possible. Total splenectomy is only done in cases where patients have severe symptoms from HS. A hematologist will determine if a splenectomy is necessary. A hematologist is a physician who specializes in diagnosing, treating and preventing blood and bone marrow diseases.
One of the major risks following a total splenectomy is a serious blood infection called sepsis. To minimize the risk of infection, your child will be given vaccinations (in addition to their routine vaccines) before the splenectomy.
After the splenectomy prophylactic (preventative) antibiotics will be prescribed to help prevent potential infections. Your child will also require booster immunizations in the years following a splenectomy. Talk to your child’s doctor to learn which immunizations will be required.
If your child has had a splenectomy and develops a fever, it is very important to see a doctor immediately to avoid overwhelming infection and serious life-threatening illness.
Because of the risks of a total splenectomy, some doctors recommend a partial splenectomy instead, even for children with severe symptoms. In a partial splenectomy only a portion of the spleen is removed. The remaining portion of the spleen will help protect against infections. Your child’s doctor will discuss the risks and benefits of a partial splenectomy.
Cholecystectomy
The gallbladder is an organ that stores and releases fluid called bile into the intestine to help with digestion of fats. Bile is partially made up of breakdown products of bilirubin. Because of the high turnover rate of red blood cells in HS, children are at risk of developing gallstones which may cause jaundice, pain, or obstruction or inflammation of the gallbladder.
If severe symptoms develop, including severe pain or inflammation of the gallbladder, the gallbladder may need to be removed. This surgery is called a cholecystectomy. If your child’s doctor and a surgeon think surgery is necessary, they will discuss the risks and benefits of a cholecystectomy with you.
Complications
Illness and aplastic crisis
Illness does not usually affect your child’s blood counts. However, some viral illnesses can worsen anemia and increase jaundice. This condition is called an aplastic crisis. Parvovirus is a common virus associated with an aplastic crisis in HS and may cause the following symptoms:
- Significant change in pallor or jaundice
- Lethargy (lack of energy)
- New onset headache (along with other symptoms listed here)
- Light-headed or dizzy
- Shortness of breath with activity
If you notice any of these signs, take your child to the doctor for a physical examination and a blood count and bilirubin test if needed. It is not necessary to check the blood counts with every illness, only if you or the doctor notice some or all of the above symptoms.
Physical activity
Generally, people with an enlarged spleen are told by their doctor to limit their activities, particularly contact sports, in order to prevent rupture of the spleen. However, the risk of splenic rupture in a person with HS is thought to be about the same as someone who does not have an enlarged spleen. As a result, your child does not need to restrict physical activity unless specifically instructed by their doctor.
When to see a doctor
Bring your child to a doctor if you notice the following signs and symptoms:
- Pale skin compared to normal colour
- Low energy (fatigue)
- Increase in yellowing of the skin and whites of the eyes
See a doctor immediately or go to the emergency department if your child has any of the following symptoms:
- Very pale or worsening jaundice
- Lethargic, inactive or difficult to wake up
- Light-headed or dizzy
- Shortness of breath with activity
- Severe stomach pain
- Headache (in addition to the above symptoms)