The most effective way to manage your child's acute pain is with a combination of physical, psychological and pharmacological (medication) strategies. Together, these are termed the 3Ps of pain control.
Like three legs of a stool, the 3Ps are complementary, or supportive, to one another. Your health-care professional can help you decide what might work best for your child.
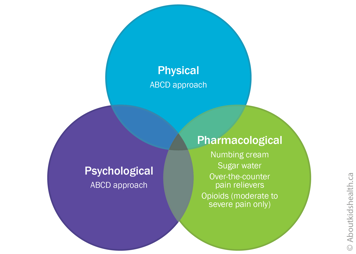
Psychological and physical strategies — ABCD approach
One helpful way to soothe your infant in pain is to use the ABCD approach. Parents have reported that it is easy to understand and a recent study shows that it helps to reduce pain in young children. If your child's acute pain is severe and lasts more than a few seconds, you can also easily combine the ABCD approach with pharmacological strategies (see below).
A: Assess your own anxiety
When you are calm, your infant or toddler is calmer and less likely to be distressed after a painful procedure or other cause of acute pain.
B: Belly breathe if you are stressed
Take a few calm and deep breaths down into your belly. This slows your own breathing and heart rate, which, if you are holding your infant in your arms, will also slow down their heart rate and breathing. When infants and toddlers are in a parent's arms, parental heartbeats and breathing can help them feel less distressed before a painful procedure. Younger children who are less distressed before a needle feel less pain afterwards.
C: Use a calm, close, cuddle with your infant
Holding your young child close, skin-to-skin if possible, reduces pain-related distress in infants. Skin-to-skin contact is also known as "kangaroo care".
- Hold your infant clothed only in a diaper and face them against your bare chest. Ideally, start this at least 15 minutes before the painful procedure, but even two minutes of contact beforehand can help. With toddlers, skin-to-skin is harder because they like to move around. Holding them close may mean holding the child on your lap.
- Sucking helps soothe a young child. Breastfeeding before, during and after a painful procedure is a powerful way to reduce your infant's pain-related distress. If you are not breastfeeding, use a pacifier before, during and after a procedure instead.
- If you cannot hold your baby, for instance because they are in an incubator or have wires connected to them, try a "hand cuddle". Your doctor or nurse may call this facilitated tucking. This involves placing your hands on your baby to help them tuck their arms and legs to their body. This approach reduces pain-related distress in pre-term infants (36 weeks gestation or less) and will also help you feel empowered.
- Another option to reduce pain-related distress when you cannot hold your baby is to swaddle them in a blanket. This provides support for your infant and stops them moving around too much. When swaddling, gently bring your infant's hands together below their chin.
D: Distract your young child
Distraction when your child's peak distress has passed (about 30 to 45 seconds after a needle, once their crying dies down) can also help ease your child's pain. Use a normal tone of voice to talk about anything other than the pain or use toys, bubbles, books and songs.
If you notice that distraction is making your child more distressed, go back to cuddling. An extra 60 seconds of cuddling can sometimes make a big difference in helping your child calm down and become more open to distraction from their pain.
Pharmacological strategies (medications)
Pain medications also minimize your infant's or toddler's pain. Always talk to a health-care professional before you use them for your child. They can advise you if the pain medication is safe and effective for your child's type of pain.
Numbing creams
Numbing creams can be helpful for painful needle-related procedures such as vaccinations. Apply the cream to the area where the needle will be inserted 30 to 60 minutes before the procedure.
Sugar water
Giving your infant just a few drops (0.1 mL) of sucrose (sugar water) right before a painful procedure can also reduce their pain.
Using a syringe or dropper, place the sugar water, one drop at a time, onto the front of your baby's tongue. You can also dip your baby's pacifier into the sugar water.
Only use sugar water when your baby is in acute pain, not when they have general irritability.
Over-the-counter medications
Giving your infant acetaminophen or ibuprofen after a painful procedure can reduce any pain that persists. These medications can also be helpful for longer-lasting acute pain like that from teething. Speak to a health-care professional if your infant is less than six months old.
Opioid medicines
Opioids are among the strongest pain relievers and are often used after surgery or other major painful procedures. If your infant is in moderate to severe pain, their health-care team may prescribe opioids such as morphine, oxycodone or hydromorphone, generally for short-term use.
| Opioids have risks and side effects, which can be serious. Always talk to your child's health-care provider for advice on taking, storing and disposing of opioids safely. |
Websites
Comforting Your Baby in Intensive Care
http://familynursing.ucsf.edu/comforting-your-baby-intensive-care
Videos
Bringin' up Baby: Soothing the Pain (3 mins 50 secs)
Psychological and physical strategies for parents to reduce vaccination pain in healthy infants
Reduce the pain of vaccination in babies(13 mins 08 secs)
Tips for parents on helping healthy infants get through vaccinations
Easing your baby's pain: A mother's story (3 mins 07 secs)
Three ways to instantly reduce your infant's pain in the NICU
The Power of a Parent's Touch (2 mins 40 secs)
How breastfeeding and skin-to-skin contact can help when an infant is experiencing a painful procedure
Content developed by Rebecca Pillai Riddell, PhD, CPsych, OUCH Lab, York University, Toronto, in collaboration with:
Lorraine Bird, MScN, CNS, Fiona Campbell, BSc, MD, FRCA, Bonnie Stevens, RN, PhD, FAAN, FCAHS, Anna Taddio, BScPhm, PhD
Hospital for Sick Children
References
Anand, K. J. S. (2012). Assessment of neonatal pain. In J. A. Garcia-Prats & M. S. Kim (Eds.), UpToDate. UpToDate: Waltham, MA.
International Association for the Study of Pain (2010) Fact Sheet on Mechanisms of Acute Pain. https://s3.amazonaws.com/rdcms-iasp/files/production/public/Content/ContentFolders/GlobalYearAgainstPain2/AcutePainFactSheets/3-Mechanisms.pdf [Accessed March 29, 2018]
Mathew, P. J., & Mathew, J. L. (2003). Assessment and management of pain in infants. Postgraduate Medical Journal, 79(934), 438-443.
McGrath, P. J. (1985). CHEOPS: a behavioral scale for rating postoperative pain in children. Adv Pain Res Ther, 9, 395.
Merkel, S., Voepel-Lewis, T., & Malviya, S. (2002). Pain Assessment in Infants and Young Children: The FLACC Scale: A behavioral tool to measure pain in young children. AJN The American Journal of Nursing, 102(10), 55-58.
Ohlsson, A., & Shah, P. S. (2015). Paracetamol (acetaminophen) for prevention or treatment of pain in newborns. Cochrane Database Syst Rev, 6(6).
Pillai Riddell, R., Lisi, D., Campbell, L. (2013). Pain Assessment in Neonates. In Encyclopedia of Pain, 2nd edition.
Pillai Riddell, R. R, Racine, N. M., Gennis H. G., Turcotte, K., Uman, L. S., Horton, R. E., Ahola Kohut, S., Hillgrove Stuart, J., Stevens, B., & Lisi, D. M. (2015). Non-pharmacological management of infant and young child procedural pain. Cochrane Database of Systematic Reviews, Issue 12. Art. No.: CD006275
Pillai Riddell, R., O'Neill, M., Campbell, L., Taddio, A., Greenberg, S., Garfield, H (2018). The ABCDs of Pain Management: A Double-Blind Randomized Controlled Trial for a Brief Educational Video for Parents of Young Children undergoing Vaccination. Journal of Pediatric Psychology. Volume 43, Issue 3, 1 April 2018, Pages 224-233, https://doi.org/10.1093/jpepsy/jsx122
Pillai Riddell, R. R., Racine, N. M., Gennis, H. G., Turcotte, K., Uman, L. S., Horton, R. E., ... & Lisi, D. M. (2015). Non‐pharmacological management of infant and young child procedural pain. The Cochrane Library.
Stevens, B., Yamada, J., Campbell-Yeo, M. Gibbins, S., Harrison D., Dionne, K., Taddio, A., McNar C Willan, A., Ballantyne, M., Widger, K., Sidani, S., Estabrooks, C., Synnes, A., Squires J., Victor, C., and Riahi, S. (2018). The minimally effective dose of sucrose for procedural pain relief in neonates: a randomized controlled trial. BMC Pediatr. 2018; 18: 85.
Stevens, B. J., Gibbins, S., Yamada, J., Dionne, K., Lee, G., Johnston, C., & Taddio, A. (2014). The premature infant pain profile-revised (PIPP-R): initial validation and feasibility. The Clinical journal of pain, 30(3), 238-243.
Stevens, B. J., Abbott, L. K., Yamada, J., Harrison, D., Stinson, J., Taddio, A., & Campbell, F. (2011). Epidemiology and management of painful procedures in children in Canadian hospitals. Canadian Medical Association Journal, 183(7), E403-E410.
Stevens, B., Yamada, J., Lee, G. Y., & Ohlsson, A. (2013). Sucrose for analgesia in newborn infants undergoing painful procedures. Cochrane Database Syst Rev, 1(1).
Taddio, A., McMurtry, C. M., Shah, V., Riddell, R. P., Chambers, C. T., Noel, M., & Lang, E. (2015). Reducing pain during vaccine injections: clinical practice guideline. Canadian Medical Association Journal, 187(13), 975-982.