Chronic pain treatments involve a mix of psychological, physical and pharmacological (medication) strategies. Together, these are called the 3Ps of pain control. Like three legs of a stool, the 3Ps are complementary, or supportive, to one another.
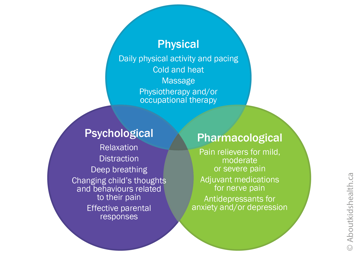
No single strategy will likely be the answer, so it is important to be open to a variety of options if your young child has chronic pain.
Physical strategies
Physical strategies are activities that help the body to function physically. They include conditioning exercises, stretches, endurance activities and nervous system retraining. They are typically guided by physical and occupational therapists.
"Pacing" is one strategy that can help an older child, once they are old enough to grasp the concept. It involves learning how to balance activity and rest so that a child can be active in important daily activities (such as participating in school and going outdoors with friends).
Try using the traffic light analogies below for your child's physical activity.
Pacing guidelines for physical activity
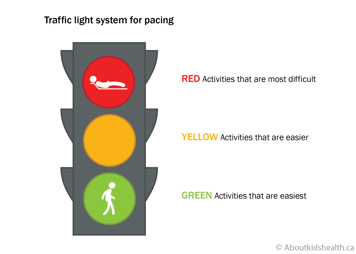
- Red light
- Severe pain increases during an activity and stops activity participation
- Pain persists for days to weeks
- Possible risk of injury
- Yellow light
- Safe pain
- Pain spikes but is tolerable during an activity and will not cause harm
- Pain persists for 24-48 hours after an activity before returning to baseline
- Green light
- Safe pain
- Pain spikes but is tolerable during an activity and will not cause harm
- Pain is no worse after an activity
Your child should stay in the green light and may edge into the yellow. They should not go in the red light.
Pacing guidelines to balance rest and activity
- Red light
- Stop and rest.
- Key phrase: “I need to take a break. I can use my coping strategies for relaxation and recovery so I am ready to go again after my rest.”
- Yellow light
- Be alert.
- Key question: “Am I overdoing it or can I use my coping strategies to keep going a bit longer?”
- Green light
- Be active but save some of your energy.
- Key phrase: “I am being active and I am fine.”
Make sure that your child has time in the green and red traffic light areas. Yellow reminds them to stop and take a break.
Psychological strategies
Psychological strategies can be thought of as "mind-body" strategies or "the power of the brain to help the pain".
In young children, psychological strategies tend to focus on behaviours rather than thoughts about their pain. Examples of behavioural strategies include:
- empowering children to make coping statements (such as "I can get through this")
- encouraging children to keep their regular routines despite their pain
- providing rewards (such as stickers or verbal praise) when they manage their pain successfully
For children aged two or three, it can be helpful to comfort them by:
- giving their favourite blanket or comfort object
- distracting them using their favourite toys or by singing their favourite song
Children aged four to five can begin seeking support from others. Encourage an older child to talk to their teacher if they need support to deal with their pain, such as a rest break or an ice pack. You might even decide on a colour system that your child can use to communicate with their teachers.
- If your child says they are in the green zone, for instance, they are feeling okay and do not need support.
- If your child is in the yellow zone, they may need some support. The teacher should be aware of this.
- If your child tells a teacher that they are in the red zone, they need support there and then.
Relaxation
Relaxation is another psychological strategy that can help your child cope with chronic pain.
Belly breathing is one such technique, as it helps your child slow down their breathing and become more relaxed. Encourage your child to take a few slow deep breaths into their belly, breathing in through their nose and out through their mouth.
They can place their hands over their belly to check that it is rising with every in-breath and falling with every out-breath.
Your child's health-care team may teach you other strategies to support your child and reduce the impact of pain on the family. These include helping to distract your child from pain, remaining calm and developing a plan to cope with pain when it arises.
Pharmacological strategies (medications)
Pharmacological strategies are the medications that treat your child's pain. They are rarely used alone; they should nearly always support physical and psychological strategies.
Pain medications are typically divided into:
- simple analgesics (pain relievers)
- opioids
- adjuvants
Simple analgesics include acetaminophen and ibuprofen and are available over the counter. They are helpful for mild to moderate pain (especially resulting from tissue inflammation).
Opioids are among the strongest pain relievers and are often used after surgery or other major painful procedures. If your young child is in moderate to severe pain, their health-care team may prescribe opioids such as morphine, oxycodone or hydromorphone, generally for short-term use.
| Opioids have risks and side effects, which can be serious. Always talk to your child's health-care provider for advice on taking, storing and disposing of opioids safely. |
Adjuvants are a group of medications shown to work well for pain but are mainly used for other reasons. Examples include anticonvulsants and cannabinoids.
For all medications, talk to your health-care professional for more information.
What kind of improvements should I see in my child's chronic pain?
Your child's chronic pain will not always improve consistently. There may be good days and bad days, good weeks and harder weeks.
Sometimes things might even get worse before they get better. For example, as your child begins their therapies and their body becomes more active, they may experience muscle soreness and throbbing. This is natural in weak or tight muscles and will ease in time.
To stay focused on managing pain effectively, make weekly goals with your child and remember that improvement can sometimes take time.
Improvements in function
One important area for goal setting is return to function. This means returning to activities that pain has disrupted, for example going to school, taking part in family routines or doing physical or social activities.
A return to function, rather than improvement in pain, is actually the first sign that chronic pain treatment is successful. This is because pain can often take weeks to months to improve while weak muscles gradually become stronger. If your child waits for their pain to go away before getting back into life, there is a risk that their pain will get worse.
Websites
Website designed to help children get control of their pain (German Paediatric Pain Centre)
http://www.deutsches-kinderschmerzzentrum.de/en/
Website where children can learn the Canadian 24-Hour Movement Guidelines the fun way https://www.participaction.com/the-science/benefits-and-guidelines/children-and-youth-age-5-to-17/
Videos
How does your brain respond to pain
https://www.youtube.com/watch?v=I7wfDenj6CQ
Video explaining what is chronic pain: Children's National Health- Sheikh Zayed Institute https://www.youtube.com/watch?v=EL1E54nH_7c
Video explaining the power of the brain and chronic pain
https://www.mycarepath.ca/understanding-pain/brain-and-nervous-system-change
Video describing pacing
https://www.mycarepath.ca/managing-pain/paced-practiced-and-increasing-activities
Sesame Street song that teaches belly breathing
https://www.youtube.com/watch?v=_mZbzDOpylA
Content developed by Danielle Ruskin, PhD, CPsych, in collaboration with:
Anne Ayling Campos, BScPT, Fiona Campbell, BSc, MD, FRCA, Lisa Isaac, MD, FRCPC, Jennifer Tyrrell, RN, MN, CNeph
Hospital for Sick Children
References
Coakley, R., & Schechter, N. (2013). Chronic pain is like… The clinical use of analogy and metaphor in the treatment of chronic pain in children. Pediatric Pain Letter, 15(1), 1-8.
Coakley, R. (2016). When Your Child Hurts: Effective Strategies to Increase Comfort, Reduce Stress, and Break the Cycle of Chronic Pain. Yale University Press.
Carney, C., Carney, C.E., & Manber, R. (2009). Quiet Your Mind & Get to Sleep: Solutions to Insomnia for Those with Depression, Anxiety, Or Chronic Pain. New Harbinger Publications.
Mindell, J.A., & Owens, J.A. (2003). Sleep problems in pediatric practice: clinical issues for the pediatric nurse practitioner. Journal of Pediatric Health Care, 17(6), 324-331.
Paruthi, S., Brooks, L.J., D'Ambrosio, C., Hall, W.A., Kotagal, S., Lloyd, R.M., ... & Rosen, C.L. (2016). Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. Journal of clinical sleep medicine: JCSM: official publication of the American Academy of Sleep Medicine, 12(6), 785.
Ruskin, D., Amaria, K., Warnock, F., & McGrath, P. (2011). Assessment of pain in infants, children, and adolescents. Handbook of pain assessment, 213-241.
Stinson, J. N., Connelly, M., Jibb, L. A., Schanberg, L. E., Walco, G., Spiegel, L. R., Tse, S. M., Chalom, E. C., Chira, P., … Rapoff, M. (2012). Developing a standardized approach to the assessment of pain in children and youth presenting to pediatric rheumatology providers: a Delphi survey and consensus conference process followed by feasibility testing. Pediatric rheumatology online journal, 10(1), 7. doi:10.1186/1546-0096-10-7
Solodiuk, J., & Curley, M.A. (2003). Pain assessment in nonverbal children with severe cognitive impairments: the Individualized Numeric Rating Scale (INRS). Journal of Pediatric Nursing, 18(4), 295-299.
Valrie, C.R., Bromberg, M.H., Palermo, T., & Schanberg, L.E. (2013). A systematic review of sleep in pediatric pain populations. Journal of developmental and behavioral pediatrics: JDBP, 34(2), 120.