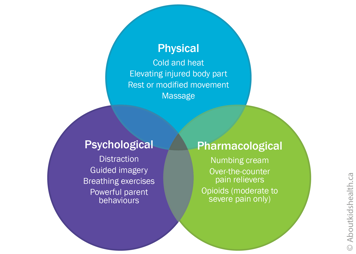
There is a lot that you can do as a parent to help your older child in acute pain. The most effective way to manage pain is with a combination of psychological, physical and pharmacological (medications) strategies. Together, these are termed the 3Ps of pain control. Like three legs of a stool, the 3Ps are complementary, or supportive, to one another.
Children aged six to 12 are going through a unique stage of development. They may be experimenting with coping by themselves, with less help from you as their parent or caregiver. Sometimes your child may want you close and holding their hand but other times want you to stand back and let them cope on their own. Do your best to learn what type of support they need and follow their lead. Ask them and be prepared for them to change their mind.
Give your older child a role in deciding how their pain will be managed by, for example, encouraging them to discover what helps them, what makes their pain worse and when they are feeling better. Your child's health-care team can also help you and your child decide which combination of the 3Ps might work best.
Psychological strategies
As a parent, you are the main source of encouragement for older children who are coping with pain. At this age, explaining to your child why they are in pain can help reduce their anxiety or worry and let them know that the pain will not last forever. You also have a role in helping your child set realistic expectations for their pain, for example by being honest about the likelihood of some pain after surgery.
Children often base their own coping strategies on the way they see you respond to painful situations. No matter how old your child, it is important to try to be calm yourself and support your child with the strategies listed below.
Distraction
Distraction can be a particularly helpful psychological strategy when a child is experiencing acute pain. Distract your child with an activity or item that interests them. Active distraction, such as doing an activity or talking, is better than passive distraction such as watching TV.
Research shows that virtual reality (VR) technology can also help distract a child during some acutely painful procedures like burn dressing changes. Relatively inexpensive options include mobile apps that your child can use with simple VR glasses or headsets.
Guided imagery
To use guided imagery, ask your child to imagine that they are in a calm, peaceful environment or to remember a pleasant experience from their past. Encourage your child to describe what they see, as well as any smells, sounds or other sensations. There are online scripts that you can print and go through with your child. You can also download online guided imagery scripts that your child can follow on a smartphone or other mobile device during a painful procedure.
Breathing exercises
Breathing exercises help your child slow down their breathing and become more relaxed. Encourage your child to take a few slow deep breaths into their belly, breathing in through their nose and out through their mouth.
They can place their hands over their belly to check that it is rising with every in-breath and falling with every out-breath.
Powerful parent behaviours
What you say, and do not say, can also influence how older children cope with pain. In fact, research has shown that not saying the "wrong" things helps your child more than saying the "right" things! The guidelines below have been shown to be very helpful.
- Do not reassure. It might sound strange, but it is better not to reassure your child when they are distressed. Telling a child, "It's ok" or "You are fine" over and over when they know they are obviously not fine (scared, crying, screaming) can actually make your child more stressed and therefore experience more pain.
- Do not criticize. Do not use your child's experience of pain to try to improve their behaviour or tell them they can do better. Saying things such as "Brave girls don't cry", "Your brother didn't cry this much" or "This needle isn't that big a deal" makes children more upset, which leads to more pain.
- Do not apologize. It is not your fault that your child is having a medical procedure, so do not say sorry for it or their pain. Some researchers believe that apologizing to your young child tells them that you are distressed. This in turn will make your child more distressed.
Decide if your child would benefit from having choices during a procedure. Young children tend to be overwhelmed by an upcoming painful procedure, so asking them is usually not helpful.
However, as children age, getting control may be helpful. If you think your child could benefit from having some control, well before the procedure (such as before you leave your home for the procedure), ask your child questions such as:
- whether they would like to have a needle in their right or left arm or leg
- where and how would they like to be positioned for the procedure
- how they want to be distracted during the procedure
- what would they like to do after the procedure
- whether they want to hold your hand
- Do tell the truth. If your child asks if a procedure is going to hurt, and you think it will, let them know it may hurt a small or medium amount but that it will be over soon. Research shows that children who are less upset before a needle show less pain after a needle.
Physical strategies
Cold and heat
If your child has any swelling or other signs of inflammation, it can be helpful to apply cold (such as a wrapped ice pack) to the area. This not only reduces signs of inflammation but can also help control pain. About 24 to 28 hours after an acute (sudden) injury, it can be helpful to apply heat (for example with a heating pad or a hot water bottle).
Be careful to avoid injury with heat and cold packs. Only apply them for short periods at a time (say, 10 minutes on/10 minutes off) and monitor the area closely. Your child should be able to move the heat or cold pack away on their own or tell you if it is uncomfortable.
Elevating the injured area
If your child has pain and swelling after an acute injury, it can be helpful to elevate (raise) the painful body part to a level above their heart. Elevating a painful arm or leg, for instance on a pillow while your child lies down, allows any excess fluid to drain. This in turn reduces pressure and pain in the injured area.
Resting or modifying movement
If your child injures themselves, it is often a good idea to rest the injured area or at least modify (change) any essential movements for a short time. This gives the injured area time to heal and protects it from further damage.
Be sure to talk to a health-care professional first because complete inactivity may sometimes increase swelling in the area and/or lead to loss of motion and muscle strength.
Massage
Massage can be a helpful form of physical therapy for acute pain caused by cramps or sports injuries.
Pharmacological strategies (medications)
Pain medications can also manage your older child's acute pain. Some children in this age group may not understand why they should take medication. You can help your child by explaining what the medication is for and how it will help them.
Acute pain medications often come in different forms (for example liquid, tablets by mouth or through a needle). If your child prefers one form of medication to another, make sure they play a key role in deciding which option is best for them.
Below is an outline of some common medications for acute pain. Because they treat different types of acute pain, some of them may be used together, if directed by your child's health-care team.
Always talk to a health-care professional before you use pain medications, especially if you are not sure which medication to use or which form of medication might work best for your child. They can advise you if a pain medicine is safe and effective for your child's type of pain.
Numbing creams
Numbing creams can be helpful for painful needle-related procedures such as vaccinations or blood tests. Apply the cream to the area where the needle will be injected 30 to 60 minutes before the procedure. Ask for directions from your pharmacist or health-care team.
Over-the-counter medications
It may also be helpful for your child to take acetaminophen or ibuprofen before or after a painful procedure. Taking these medications 30 to 40 minutes before a procedure is sometimes recommended.
These medications can often last four to six hours, so can be particularly good for acute pain such as an earache or pain after an injury.
Opioid medications
Opioids are among the strongest pain relievers and are often used after surgery or other major acute painful procedures. If your older child is in moderate to severe acute pain, their health-care team may prescribe opioids (such as morphine, oxycodone and hydromorphone) for short-term use.
| Opioids have risks and side effects, which can be serious. Always talk to your child's health-care provider for advice on taking, storing and disposing of opioids safely. |
Websites
Faces Pain Scale-Revised
https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1519
Pain Management During Immunizations for Kids and Adolescents
https://immunize.ca/pain-management-kids-and-adolescents
Managing your child's pain from braces
https://1stfamilydental.com/reducing-braces-pain/
Managing your child's pain from sports injuries
http://www.stanfordchildrens.org/en/topic/default?id=tackling-kids-sports-injuries-1-4288
Preparing your child with cancer for painful procedures
http://www.cancer.net/navigating-cancer-care/children/preparing-your-child-medical-procedures
Page designed for children and youth to discuss their medication with their health-care provider
Five Questions to Ask About My Medicine
Videos
Pain management at SickKids (2 mins 49 secs)
https://www.youtube.com/watch?v=_9_OQFo2APA
Reducing the pain of vaccination in children (Centre for Pediatric Pain Research) (2 mins 18 secs):
https://www.youtube.com/watch?v=KgBwVSYqfps
Reducing the pain of vaccination in children (Dr. Taddio) (20 mins 52 secs):
https://www.youtube.com/watch?time_continue=2&v=TGGDLhmqH8I
Learning how to manage pain from medical procedures (Stanford Children's Health) (12 mins 58 secs)
https://youtu.be/UbK9FFoAcvs
Content developed by Rebecca Pillai Riddell, PhD, CPsych, OUCH Lab, York University, Toronto, in collaboration with:
Lorraine Bird, MScN, CNS, Fiona Campbell, BSc, MD, FRCA, Bonnie Stevens, RN, PhD, FAAN, FCAHS, Anna Taddio, BScPhm, PhD
Hospital for Sick Children
References
Gold, J.I., Mahrer, N.E. (2017) Is Virtual Reality Ready for Prime Time in the Medical Space? A Randomized Control Trial of Pediatric Virtual Reality for Acute Procedural Pain Management. Journal of Pediatric Psychology, 2017; https://doi.org/10.1093/jpepsy/jsx129
Jaaniste T, Hayes B, von Baeyer CL. Providing children with information about forthcoming medical procedures: A review and synthesis. Clinical Psychology: Science and Practice, 2007;14(2): 124-143
McMurtry, C.M., Chambers, C.T., McGrath, P.J., & Asp, E. (2010). When "don't worry" communicates fear: Children's perceptions of parental reassurance and distraction during a painful medical procedure. Pain, 150(1), 52-58.
Taddio, A., McMurtry, C.M., Shah, V., Pillai Riddell. R. et al. Reducing pain during vaccine injections: clinical practice guideline. CMAJ 2015. https://www.cmaj.ca/content/187/13/975
Uman, L.S., Birnie, K.A., Noel, M., Parker, J.A., Chambers, C.T., McGrath, P.J., Kisely, S.R. (2013) Psychological interventions for needle-related procedural pain and distress in children and adolescents. Cochrane Database of Systematic Reviews https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD005179.pub3/full
von Baeyer, C.L. (2009). Children's self-report of pain intensity: what we know, where we are headed. Pain Research and Management, 14(1), 39-45.