What is a cataract?
A cataract is a cloudy area over the lens of the eye. Cataracts can affect one or both eyes. Childhood cataracts are rare: they occur in one to three in 10,000 children.
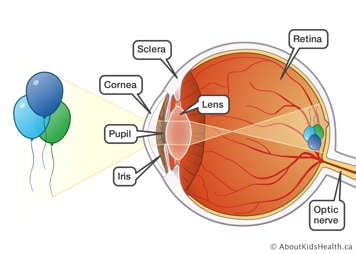
A healthy eye
The eye is like a camera. It records pictures of what it sees. But to see clearly, all parts of the eye must work properly.
- The cornea is a clear outer covering at the front of the eye. It covers the iris and pupil.
- The sclera, or white part of the eye, is the continuation of the cornea around into the back the eye.
- The iris is the coloured part of the eye and controls how much light enters through the pupil.
- The pupil is the window in the centre of the iris.
- The lens is behind the pupil. It is designed to focus the rays of light onto the retina, just like a camera lens focuses an image onto a film.
- The retina is the innermost covering of the eye. It converts the rays of light into an electrical signal and sends the signal to the brain.
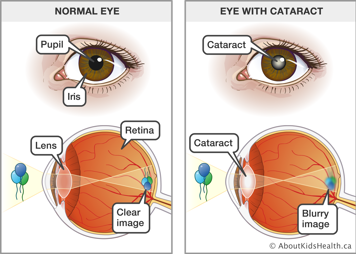
What happens when your child has cataract(s)
When your child has a cataract, the lens cannot focus the rays of light onto the retina normally. Instead, the lens produces blurry images, which reduce the child's vision.
Your child's vision might be mildly or seriously affected by a cataract, depending on how big it is and where it covers the lens. A cataract will not affect your child's vision if it is very small or away from the centre of the lens.
Causes of cataract
A cataract can be congenital (a person is born with it) or can be acquired or developmental (it appears later in childhood or in adulthood).
Common causes include:
- heredity (inheriting a cataract from a parent)
- trauma (injury) to the eye
- radiation (treatment for cancer)
- medication (for example steroids)
- other illnesses or conditions (for example Down syndrome)
- infection (for example German measles).
In many cases, however, the cause of a cataract is not known.
How to tell if your child has a cataract
Have your child's eyes examined by an ophthalmologist (say: op-thal-MOL-o-jist), a medical eye doctor, if:
- you notice a white spot on your child's eye(s)
- a parent or sibling had a cataract as a child (not as an older adult)
- your child has eye problems or another disease or condition in which cataracts are likely to be present
- your family doctor or paediatrician recommends an eye exam because of a concern about possible cataracts
- your child's eyes are crossed
- there is a concern about your child's vision.
If there is a family history of cataracts in childhood, bring your child to an ophthalmologist before they are two weeks old.
Checking your child's eyes for cataracts
The ophthalmologist will carefully examine your child's eyes. Here is what you can expect during the exam.
- Your child will have special eye drops to make their pupils bigger. These drops sting at first but only for about 10 seconds. They may be repeated.
- Since your child needs to be very still when the eyes are checked, they may be wrapped in a blanket and held down gently, especially if they are very young or too upset to stay still on their own.
- When the drops start to work, usually after about 30 minutes, the ophthalmologist will shine a bright light into your child's eyes and use different instruments to help check them.
Being held down and having a bright light shone in their eyes will make your child uncomfortable, but they should not feel any pain.
After the exam, the eye doctor will explain the condition of your child's eyes. If there is a cataract, the doctor will tell you and talk to you about the best treatment for your child.
Treatments for cataracts
Cataracts do not go away by themselves, except in a few rare situations.
Mild cataract
If the cataract is small and does not affect your child's vision, the doctor may decide not to treat it at all or may prescribe special eye drops to dilate (widen) the pupil to allow more light to enter the eye. If your child needs eye drops, make sure you carefully follow the instructions for putting them in.
Serious cataract
If the cataract is more serious, your child will need surgery to remove it. Cataracts cannot be removed with medication or lasers.
Why it is important to have surgery to remove a serious cataract
Surgery is important because it will allow your child's vision to develop as normally as possible. It is especially important for children aged under nine because their vision is still developing.
If your child has a cataract and they are aged under nine, there is a risk that they will develop amblyopia if the cataract is not removed. Amblyopia is sometimes called "lazy eye" and can occur when the affected eye does not get enough stimulation from light rays.
All children aged under nine should be operated on as soon as possible, whether they are born with a cataract or develop one later. If your child develops a cataract when he is aged nine or over, the timing of the surgery is more flexible because their vision has fully developed.
What happens during cataract surgery
Before the surgery, your child will have special drops to dilate (widen) the pupil of the eye. These drops sting at first but only for about 10 seconds. They may need to be repeated once or twice.
The eye drops are usually applied right before the surgery in the hospital. If your child needs them before then, your eye doctor will give you a prescription for the drops and explain when to start putting them in.
Your child will have a special "sleep medicine" called a general anaesthetic for the surgery. This will make sure they sleep through the operation and do not feel any pain.
The surgeon takes out the cataract by removing the lens of the affected eye(s). Your eye doctor will tell you before the surgery if it is best to remove the whole lens or only part of it.
The surgeon will use special stitches to repair the eye wound. These stitches are absorbable, meaning that that they do not need to be taken out. They will dissolve on their own over the first six to eight weeks after surgery.
In young children with cataracts in both eyes, surgery is often done on the second eye as soon as possible after the first eye. This is to make sure that the vision in both eyes develops evenly.
At times, surgery may be done on both eyes on the same day. Your eye doctor will explain exactly when your child will have surgery and, if it applies, when each eye will be done.
The operation is usually done as a day surgery if your child is over 12 weeks old. If your child was born prematurely or if the surgery is within the first 12 weeks of life, they will usually stay in the hospital overnight.
What to expect after the surgery
Eye patch and shield
Immediately after surgery, an eye patch will be placed over the operated eye. The eye patch is covered with a plastic or metal shield for protection. Your child's patch will be removed the next day by the ophthalmologist when they return to the eye clinic. If the patch comes off at home, you can leave it off, but make sure you put the eye shield back on.
Your child will continue to wear the shield over the operated eye to protect it while they are sleeping. Your doctor will tell you when your child can stop wearing the shield.
Pain or discomfort
Your child may experience some pain or discomfort in the operated eye. Please ask your doctor what medication you can give your child at home to relieve the discomfort or pain.
The nurses in the recovery room will watch your child for signs of pain or discomfort and will be able to give medication if your child needs it.
Before your child is discharged from hospital, please ask the nurse when your child last had any pain relief medication. This way, you can monitor your child's pain and give medication safely as needed.
Redness, swelling, and discharge
The operated eye will be red and slightly swollen after the surgery. It will also produce a clear discharge. These should decrease over the next few days.
Blurred vision
Without the lens, your child's eye is no longer able to focus clearly, but be assured that your child will not be blind. Objects will be very blurry at first until your child receives a corrective device to improve their vision. You can read more about corrective devices below.
How to care for your child after cataract surgery
Antibiotic and cortisone drops
Sometimes the doctor will order antibiotic drops or a combination of antibiotic and steroid drops for the operated eye(s). Your child may also need to have eye drops or ointment to keep their pupil dilated. If your child needs eye drops, your child's doctor will let you know. Please follow any instructions for applying the ointment or putting in the eye drops correctly.
Day-to-day activities
The surgeon who operated on your child will give you instructions about how else to care for your child after surgery. You will need to know, for example, how soon your child can return to normal activities, whether they can have a bath or a shower and when they can return to school or day care.
Use this section to write down the instructions from the surgeon.
Allowed activities:
____________________________________________________________________
Swimming:
____________________________________________________________________
Bath or shower instructions:
____________________________________________________________________
When your child can return to school or day care:
____________________________________________________________________
Other questions you want to ask:
____________________________________________________________________
Long-term effects of cataract surgery
Scar tissue or slight cloudiness
Cataracts do not re-appear after surgery, but sometimes the lens capsule may develop scar tissue or slight cloudiness. If this happens, your eye doctor will explain how it will be treated.
Other eye conditions
Even after patching, and being fitted with a corrective device, your child may develop other eye conditions after surgery. These include strabismus, inflammation (irritation or swelling), glaucoma and retinal detachment.
You will need to take your child for regular check-ups to let the eye doctor monitor your child's vision closely and check for any of these conditions as early as possible. It is important to keep all your follow-up appointments.
If you have any questions or concerns, please call your child's eye surgeon. Please write the surgeon's name and phone number here.
Doctor: ________________________ Phone: _________________________
When to call your doctor
Call your doctor immediately if:
- your child feels more pain or sensitivity to light
- your child's eyelid becomes redder or more swollen from day to day
- your child complains of or shows any signs of decreased vision
- there is any yellowish or greenish discharge from the eyes
- your child shows any other changes that concern you
Follow-up appointments after cataract surgery
Follow-up appointments are as important as the surgery itself. These appointments are usually scheduled:
- one day after surgery
- one week after surgery
- four weeks after surgery
Every time the eye doctor sees your child, they will tell you when to come back again.
It is very important to keep these appointments.
Write the date and time of the first appointment here: ______________________
Corrective devices after cataract surgery
A corrective device is something that your child wears to repair their vision. Before the surgery, your child's ophthalmologist will discuss the best device for your child. The main options are:
- contact lens
- intra-ocular lens
- eye glasses.
Your child's eye may also need to be patched. Patching is described in the next section.
Contact lens
A contact lens is an artificial lens made of special material, which can be either soft or hard. It is placed on the child's eyeball.
Once your child's eye has healed enough, they will be fitted for a lens, usually in the eye clinic. Sometimes a child will need to be sedated (calmed with medicine) for the fitting or may even need a general anaesthetic.
The eye doctor will start the fitting by putting an anaesthetic drop in the operated eye.
The doctor will then place a sample contact lens on the eyeball and measure the child's contact lens prescription for strength and fit. Your doctor will explain the strength of contact lens your child is prescribed and the reason for it.
The eye doctor or your optician or optometrist (where you buy the contact lens), will teach you how to insert and take out the contact lens as well as how to clean and store it. Make sure you understand these instructions.
Your child's vision will need to be checked regularly (by an ophthalmologist) with the contact lens on. Because your child's eyes are still growing, they will get a new prescription to adjust the contact lens strength and fit.
Younger children may be prescribed glasses to wear as a back-up when not using the contact lens. Older children may need glasses or bifocals in addition to their contact lenses.
Although it might seem like a major change, babies and children adjust to contact lenses more quickly than adults do.
Intra-ocular lens
An intra-ocular lens is an artificial lens placed in the eye. Most times this is done during the surgery to remove the lens, but it can sometimes be done later. If your child needs this type of lens, the doctor will tell you when it will be fitted.
Unlike the normal lens in the eye, an intra-ocular lens does not change its focusing power. Your ophthalmologist will decide what power of intra-ocular lens your child needs.
Your child may also need bifocal eye glasses. Your doctor will discuss this with you.
Eye glasses
Eye glasses are prescribed only if no other device is suitable. This because the lenses are thick and would distort, or interfere with, your child's vision and the glasses feel heavy to wear. However, the vision will develop with glasses just as well as with another corrective device.
If a baby needs eye glasses, the prescription will be for near vision, as they spend their waking hours focusing on things up close (for example food, toys or a parent's or caregiver's face).
When the baby gets older and needs distant vision, they will get a prescription for bifocals (lenses that allow the eyes to focus on things that are close and far away).
Remember to have regular check-ups
Whatever corrective lens is prescribed, your child will still require regular check-ups with the ophthalmologist. Please call your eye doctor between appointments if your child develops:
- any discomfort or pain
- discharge, redness or swelling of the eye
- decrease in vision
- any unusual signs or symptoms.
Eye patching
When a child has cataract(s), the vision in the affected eye does not develop properly, which can lead to amblyopia.
If there is any difference in vision between the eyes, even if both eyes were operated on, the doctor will order an eye patch. Blocking the vision of your child's stronger eye with a patch will help to strengthen the weaker eye.
If your child's eye needs patching, your eye doctor will explain:
- which eye needs to be patched
- how long and how often your child should wear the patch
- when a follow-up appointment is needed to check your child's vision.
At SickKids
If the eye doctor who operated on your child's eye(s) is not available, call 416-813-7500 and ask for the eye doctor on call.