What is a pacemaker?
A pacemaker is a small device that uses electrical impulses to control the speed and rhythm of your child's heartbeat.
How does the normal heart work?
The heart is a pump that moves blood through your body. The rate and rhythm of the heartbeat are normally controlled by the heart's own natural electrical system. The upper portion of the heart has its own pacemaker, called the sinus node. Electrical impulses start in the sinus node and travel down through the atria (upper chambers), causing them to contract. The impulses then reach the place where the atria join the ventricles (lower chambers).
This place is called the AV node. The AV node sends the impulses through the muscles of the ventricles, causing them to contract. When the ventricles contract, they pump the blood out of the heart to the rest of the body.
For more information, please see How the Body Works: Electrocardiogram (ECG).
Why does my child's heart need a pacemaker to work normally?
There are several reasons why a child might need a pacemaker. The two main reasons are heart block and sick sinus syndrome.
- Heart block: With heart block, the electrical impulses do not pass normally between the upper and lower chambers because of a blockage at the AV node. This blockage can exist before birth (congenital heart block) or can result from surgery to repair a cardiac defect. Acquired heart block can result from heart infections (such as endocarditis or myocarditis) or even from certain drugs.
- Sick sinus syndrome: In sick sinus syndrome, the sinus node does not work properly. The result is that the heartbeats are too slow or too fast.
How does the pacemaker work?
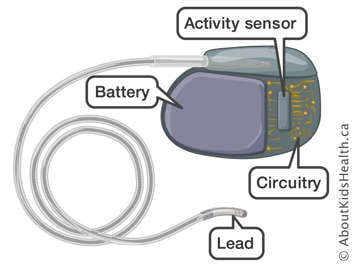
The pacemaker has two parts: the pacemaker itself and the lead (wire).
- The pacemaker: This is a small metal container that holds the battery and electrical circuits. It is very small, weighing less than two ounces. It is placed under the skin and muscle, either near the shoulder or near the stomach area. The pacemaker watches for the natural electrical activity of the heart, and sends electrical impulses to make the heart beat only when necessary.
- Leads: The electrical impulse from the pacemaker travels through insulated wires with metal tips called leads that are in contact with your child's heart. Depending on the type of pacemaker, the leads may be attached to the upper chamber of the heart, the lower chamber, or both.
Pacemaker infection
Pacemaker pocket infection can be a serious complication. It is important to recognize it and manage it early. In the post-operative period, look at the incision site(s) every day. Call the pacemaker clinic if you notice any increasing redness, swelling, tenderness, pus oozing from the incision site(s) or persistent fever. Your child should wear loose comfortable clothing to avoid irritation of the incision site(s).
Lead dislodgement
A risk with a transvenous pacemaker is that the lead dislodges from the correct placement. To help prevent this from happening, the arm on the affected side should not be raised higher than shoulder height for 8 weeks after implant.
What kinds of pacemakers are available?
Pacemakers come in many different makes and models. Your child's doctor will decide which kind of pacemaker your child should have. For more information about pacemakers, you can talk to your doctor or the pacemaker clinic staff.
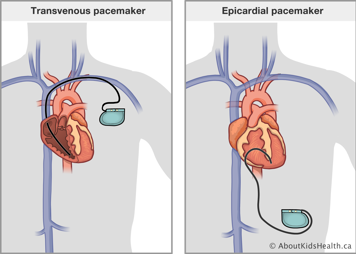
Transvenous vs. epicardial pacemaker systems
In children, pacemakers can be placed in one of two ways:
- The pacing lead can be attached to the inside surface of the heart and the pacemaker is placed in the shoulder area. This is called a transvenous pacemaker system.
- The pacing lead can be attached on the outside surface of the heart and the pacemaker is placed in the abdomen. This is called an epicardial pacemaker system.
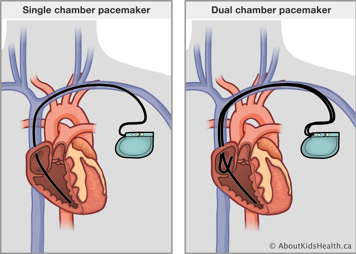
Single vs. dual chamber pacemakers
A single chamber pacemaker system has one pacing lead that is placed either in the top (atrium) or the bottom (ventricle) chamber of the heart. A dual chamber pacemaker has two pacing leads, with one lead each in the top and bottom chambers of the heart.
Rate-responsive pacemakers
Pacemakers can adjust the pacing rate according to the level of the patient's activity. For example, most pacemakers have built-in sensors that can detect body motion such as walking or running and increase the pacing rate in proportion to the patient's activity.
Read this article about pacemaker surgery to learn more about the procedure.
After the pacemaker surgery, your child will need an ECG, a chest X-ray and Holter monitor to confirm the pacemaker settings are correct. Patient’s typically stay one night in the hospital for pain management and monitoring. Before your child is discharged, you will receive teaching on how to care for the incision site and precautions about the pacemaker. Your child’s first follow-up appointment in pacemaker clinic will be 4 to 6 weeks after the surgery.
Your child should avoid strong electric and magnetic fields
Strong magnetic fields will temporarily interfere with the pacemaker's ability to sense the heart's activity. When this happens, the pacemaker will respond by sending out its pacing impulses at a fixed rate. It will not turn itself off. Your child needs to take precautions with the following:
- If your child visits the Hydro exhibit at the Ontario Science Centre, they should stay behind the rope because the strong magnet can interfere with the pacemaker.
- If your child has Industrial Arts classes at school or is interested in mechanical hobbies, they should not work with arc welders or alternators.
- Any procedure involving electrical equipment that is used in a doctor's office or an operating room may interfere with the pacemaker's function or change the pacemaker's settings. An example is electrocautery, which uses electricity to burn (cauterize) tissue.
- The pacemaker system may or may not be magnetic resonance imaging (MRI) compatible depending on the make and/or model. An MRI request should always indicate that the patient has a pacemaker and the request will be reviewed by the pacemaker team. If the pacemaker is MRI compatible, a pacemaker check will need to be performed before and after the MRI.
- Items containing magnets, such as magnetic jewelry, toys with large magnets, and some headphones should be kept at least six inches away from the pacemaker.
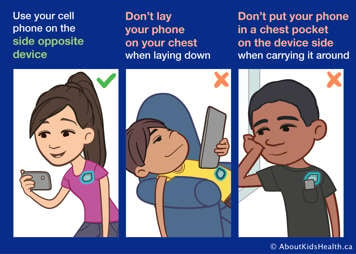
- In general, any electronics should be kept at least six inches away from the pacemaker. An example is a cellphone.
- Your child should walk through anti-theft detectors normally and should not linger between the gates. The pacemaker may activate the alarm but should not be affected by it.
Activity
Most children with a pacemaker can play and work normally, but there are a few precautions. Your child should avoid contact sports that may cause repetitive, direct impact to the pacemaker, such as karate, kickboxing or rugby. Repeated blows could weaken or damage the leads. The pacemaker clinic staff will discuss these precautions with you and your child.
Your child's cardiologist will discuss with you any other activity restrictions that are related to your child's underlying heart condition.
How often must the pacemaker be changed?
The pacemaker battery is reliable and the battery level goes down very gradually. The pacemaker battery information is obtained at each routine pacemaker clinic visit. The pacemaker is replaced when the battery reaches the replacement level. At this level, there is still a two- to three-month window where the pacemaker continues to work properly. This allows time for the doctor to book the surgery electively.
In general, a pacemaker may last between five and 12 years depending on how often it is being used, how much energy is used for pacing and the make and/or model. Surgery may be done sooner if there are problems with the pacing lead wire(s) or the pacemaker system. Your child will be admitted to the hospital for about a two-day stay to have the surgery to replace the pacemaker.
What happens in the pacemaker clinic?
Clinic staff will check your child's pacemaker by using a small computer. The pacemaker's settings, such as heart rate, can be changed using this computer. Your child will not feel any discomfort or pain during this procedure.
Chest X-rays may be taken if the cardiologist thinks there may be a problem with a lead.
In addition, a Holter monitor will be used if your child is experiencing symptoms or pacemaker settings are changed. This allows the cardiologist to check the pacemaker's functions.
Follow-up appointments
Attend all appointments at the pacemaker clinic, which typically occur every 6 months. The appointments are more frequent after a pacemaker surgery. Your child will also have regular visits with a cardiologist. Regular medical follow-up is very important.
When the battery is starting to get low, some follow-up may be done over the telephone using a monitoring device called a telephone transmitter. This method is helpful, but it does not replace regular clinic visits.
Who to call if you have questions
If you are concerned about your child, please seek medical attention. Call your child's primary health-care provider, or call 911 as needed. You may also call the pacemaker clinic staff if you have any specific questions about the pacemaker.
Pacemaker settings
You should be aware of your child’s pacemaker settings. Depending on the settings, they will have a low rate and an upper rate. If the pacemaker is programmed to prevent the heart rate from going too low, your child’s heart rate should never be slower than the programmed low rate. If you notice that the heart rate is too low and your child has no symptoms, please call the pacemaker clinic. If the heart rate is too low and your child has symptoms, please go to the nearest emergency department.