What is atopic dermatitis (eczema)?
Atopic dermatitis is a chronic (long-lasting) skin condition that comes in many forms. Some children may have very mild eczema, while others may have a severe form. Sometimes, as children with eczema grow older, their symptoms lessen or disappear altogether. Other children may have eczema for life.
With eczema, the skin becomes dry, very itchy and a rash may appear. There are times when the condition is worse and times when the condition is better. When the condition worsens, this is called a flare-up. Flare-ups often occur in certain seasons, such as in the winter months when the air is drier for some children and in the humid summers for other children. However, flare-ups can happen any time throughout the year.
The causes of eczema are unclear. Both genetic and environmental factors likely play a part. Children who have eczema may also have asthma or allergies such as hay fever.
There is no cure for eczema, but your health-care team will work with you to develop a plan to control the symptoms. They will also work with you so that you recognize when your child needs to see a health-care provider.
Signs and symptoms of eczema
Signs and symptoms may vary depending on how severe your child’s eczema is.
Signs and symptoms of eczema include:
- dry skin
- redness
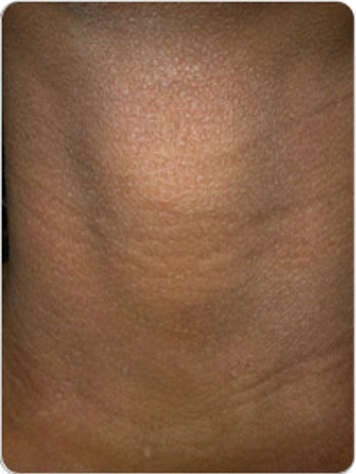
- eczema patches (scaly rash that may have redness or be the same colour as your skin)
- thickening of skin
- scratch marks
- skin colour changes (lighter or darker than your normal skin colour when the rash is gone; this heals up)
- oozing of clear fluid, crusting ("scabs")
- itching (pruritus)
- sleep loss (from itching at night)
- discomfort from scratching
- pain from open wounds


How to manage eczema
Good skin care, including moisturizing, is a key part of managing your child's eczema.
It is sometimes possible to figure out what factors cause flare-ups in your child. If you know the triggers of your child's eczema, help your child stay away from them. However, many flare-ups happen without an obvious trigger.
Your child’s health-care provider may also prescribe one or more medicines to help your child. These medicines may be topical (applied to the skin) or oral (to be taken by mouth).
Skin care
Bathing
Gentle bathing techniques are recommended, such as:
- Limiting baths to warm (not hot) water for about five to 10 minutes. Hot water can irritate the skin and trigger itching. If you need a reminder, try using a timer.
- Some health-care providers may recommend bathing frequently to help with eczema, and some may recommend bathing infrequently. Neither of these methods has been shown to be better than the other.
- If you use soap to cleanse the skin, avoid any product that irritates (stings or hurt) the skin or causes itching. Most children who bathe in warm water will have their skin look redder while in the bath and for a while after. This is from the warm water bringing more blood flow to the skin. If it is accompanied by increased itching, it could be a sign that the warmth of the water or the bath product aggravated the eczema.
- Do not use wash cloths, sponges or loofahs to scrub or rub the skin as these can cause irritation when rubbed along the skin.
- When you have finished bathing your child, pat their skin dry—do not rub.
- After bath time, apply your child's medication, then apply a layer of the prescribed medicated ointments or creams to all the affected skin areas (the rough, red, bumpy and itchy spots).
- After applying the prescribed active ointment or cream, use a product like petroleum jelly or moisturizer over the unaffected skin areas.
- Use bath time as a chance to inspect your child's skin for irritation or flare-ups.
- Children should never be left in a bath unattended.
Moisturizing
Dry skin is one of the most common features of eczema. When skin is dry, it can be itchy. It also starts to lose its function as a protective barrier. This means that more water is lost from the skin, and irritants can get into the skin. Both can trigger an eczema flare-up.
Moisturizers help decrease the itch and soothe the skin. They do this by creating a protective layer over the skin that acts as a barrier. This helps keep the water in the skin and the irritants out. Moisturizers are a mixture of fats, oils and water. There are three kinds of moisturizers that are used: ointments, creams and lotions.
- Ointments are thicker, greasier products. Most of them do not contain water. They are the most effective method for hydrating very dry skin and large areas of skin. They are usually well tolerated.
- Creams are a mixture of fats and water. They feel light and cool on the skin. Creams are used very often to prevent skin from drying out and when skin is cracked. These products often "burn" or sting the skin of patients with eczema.
- Lotions contain the most water. They spread easily and can be cooling to the skin. They can be used on the scalp. They are not as effective for moisturizing dry skin as ointments or creams. Lotions can cause skin discomfort or stinging in very dry skin.
Avoid any product that irritates the skin. No particular brand of moisturizer is better than another. Find one that works well and that your child likes.
Medicines and other treatments
Depending on how severe your child's eczema is, your child's health-care provider may prescribe one or more medicines.
Topical corticosteroids
Topical corticosteroids are steroid ointments or creams ("cortisones") that are put on the skin. Steroids are an effective way to help reduce inflammation in the skin. Inflammation causes swelling, redness, bumpiness and skin irritation. Less inflammation leads to less itching and, therefore, less scratching.
These medicines are grouped by strength. Which corticosteroid you use depends on where the flare-up is on the body and how bad it is. For example, your child might need a milder corticosteroid for the face but a stronger one for the body. Your child's health-care provider will explain which type is best for your child. By carefully following your health-care provider’s instructions, you will use topical corticosteroids in the optimum way. This will allow for a better control of your child's flare-ups. When used correctly, topical steroids rarely have side effects. If you have concerns about these medications, talk to your health-care provider about them.
Topical calcineurin inhibitors
Topical calcineurin inhibitors are non-corticosteroid medications that help treat the inflammation in the skin. They are applied directly to the affected area of skin. Their brand names are Protopic and Elidel. These medicines are used in:
- children who cannot tolerate topical steroids
- children whose eczema does not improve as much as expected with proper use of topical steroids
Other non-corticosteroid topical treatments
Crisaborole is a non-cortisone anti-inflammatory medication sometimes used for eczema. This is usually used two times a day for flares.
Anti-infective agents
Having eczema increases a person's risk of skin infection. Scratching can disrupt the skin barrier, making it easier for bacteria on the skin to enter the body and cause infection. Viruses or fungi can also cross the skin barrier, although this is less common. Infection in the skin can make eczema worse.
Anti-infective agents are medicines used to fight infections caused by bacteria (antibiotics), viruses (antivirals) and fungi (antifungals). If your child needs an anti-infective, your child's health-care provider will prescribe one.
Coal tar preparations
Crude coal tar can be used to treat skin inflammation and soothe itch. This treatment has many ingredients that have not all been identified but seem to help. Many people avoid using this treatment because it can be messy, it has some odour, it can take a lot of time and it is not very convenient.
Herbal remedies and alternative therapy
Herbal remedies and alternative therapy may include the use of:
- herbal and dietary supplements
- vitamins
- other over-the-counter products
These products have not been proven to help with eczema. Tell your health-care provider about any alternative therapies and supplements your child is using.
Managing the itch
Here are some tips that you and your child can use to help control the itching of eczema:
Tips for moisturizing
- Moisturize, moisturize, moisturize!
- Keep moisturizers and medicines cool by storing them in the fridge.
- Avoid products that contain irritating ingredients such as alcohol and fragrances (perfumes).
- Try applying a cool washcloth followed by moisturizing the skin.
Clothing tips
- Have your child sleep with one layer of loose cotton pajamas because sweat can irritate the skin.
- Avoid bedding and clothing with fabrics that irritate your child's skin. Some that might be irritating include nylon, wool or other rough fabrics. Cotton is often well tolerated.
- Cut off the tags on clothing as these can sometimes irritate the skin.
Tips for reducing scratching
Scratching is a sign of a flare-up in children with eczema and indicates that your child's eczema could be better managed. Try the following suggestions. If the scratching goes on, ask your child's health-care provider for advice.
- Ensure you are using your prescribed medications at the very first sign of a flare-up (or flare) and continue to use it until the flare is gone. "Under-treating" a flare (starting to treat the flare-up when it's already bad and stopping as soon as it's a little better but not gone) can lead to chronic itch. It can be frustrating as it seems the medicines are not working. The medicines work when the entire flare is treated, leaving the skin clear. Another flare may come, but there should be some "clear" time between flares. If a flare has not gone away within three weeks, your child should see their health-care provider.
- Use a washing cloth cooled with cool water when your child feels itchy to help decrease scratching. Avoid using a washing cloth on large parts of the body because it may cause heat loss in babies and small children.
- Keep your child’s fingernails short.
- Ask your child to tell you when they are itching. Itching is the sign that your child's eczema is not under control. Itching leads to scratching. This leads to further irritation and inflammation and makes the condition worse.
- If you notice that your child is often scratching at a particular time of day, assume it is the start of a flare-up and begin treating those areas even if there is no rash.
- Antihistamine medications do not effectively reduce the itch in children with eczema and are not routinely recommended.
Tips for managing your child's environment
- If heat or humidity is a trigger for your child, keep the environment cool but not cold. Young babies cannot control their temperature well and should be in environments between 20°C and 22°C. Fans may help but should be placed safely out of reach of children.
- It is better for your child if they sleep alone. When a child is sleeping in the same bed as others, this can lead to flare-ups because the heat created by the other bodies increases and makes your child sweat more. Do not share a bed with your baby. It increases the risk of sudden infant death syndrome (SIDS).
- Stress can sometimes cause increased scratching. Strategies such as deep breathing and mindfulness can be helpful for managing stress in children and teens. To learn more about mindfulness and find guided audio meditations, please see AboutKidsHealth's mental health video playlist.
Other considerations
Seasonal changes
You may find that your child's
eczema is worse in the colder, drier months. During this time, the air becomes very dry and holds less moisture. This can cause drier skin. In the warmer months, the humidity can also worsen eczema for some people.
Laundry care
If a laundry product you are using seems irritating, consider trying a gentler product. Some families find gentle laundry products cause less irritation of the skin.
Coping with eczema
The daily care routine for eczema can be very stressful to you, your child and the rest of your family. It is very important to maintain the routine and be committed to it to manage your child's eczema. Your child's health-care team is a good resource if you need advice. Some children develop self-esteem problems or feel embarrassed by their eczema. That is one of the reasons why it is important to keep your child's eczema under control.
School and activities
If your child goes to daycare, talk to the daycare staff and to parents of other children that attend the daycare about eczema. Inform them about your child's condition and that it will not spread to other children.
If your child needs daytime moisturizing, have a doctor's note allowing your child or a nurse to apply it at school.
School can cause a great deal of stress in children with eczema. Parents, family members and teachers should understand the stress that these children experience and that they may need more emotional support and understanding.
It is important that your child is able to participate in their regular activities as much as they can. You may be able to make some changes to help enable this.
When your child should see a health-care provider
Contact your child's health-care provider in the following situations:
- When you start treating a patch of eczema as prescribed but find no improvement after a few days.
- When medicines used as directed have started to help a patch of eczema, but the area is not clear within three weeks.
- If you see any sign of infection, such as crusting ("scabs"), oozing, pus or blister.
