To learn about celiac disease through an interactive eLearning module, click the play button below.

What is celiac disease?
Celiac disease can affect people of all ages anywhere in the world. In people with celiac disease, any contact with gluten (a family of food proteins) triggers a reaction from the body’s defense (immune) system. This immune response to gluten causes damage to the gut (small intestine) lining. This is why celiac disease is called an autoimmune disease.
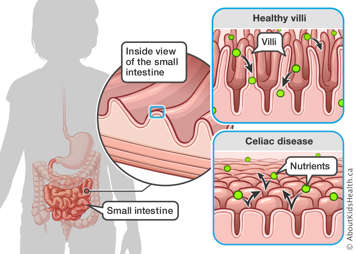
A healthy small intestine is lined with tiny finger-like projections, called villi, that stick up from the surface. Villi increase the area available to absorb nutrients from food. When children with celiac disease are exposed to gluten, the resulting immune reaction damages villi, which become flat. As a result:
- This may affect the absorption of nutrients. This is called malabsorption.
- A lack of nutrients may affect growth and development.
- It also may cause symptoms of celiac disease, such as diarrhea, constipation and stomach pain.
What is gluten?
Gluten is the common name of a family of proteins found in grains that cause the intestinal damage in celiac disease. Gliadin and glutenin are the two main gluten proteins.
Gluten is found in:
- all forms of wheat (including durum, semolina, spelt, kamut, einkorn and farro)
- wheat hybrids (including triticale which is a mix of wheat and rye)
- rye
- barley
Signs and symptoms of celiac disease
Some people with celiac disease may have no symptoms at all.
However, many people with celiac disease experience a range of symptoms. When a person with celiac disease is exposed to gluten, they may have trouble with their gastrointestinal system, malabsorption-related issues and other symptoms. Below are some common symptoms of celiac disease. Some people may only have one of these symptoms, while others may experience multiple symptoms.
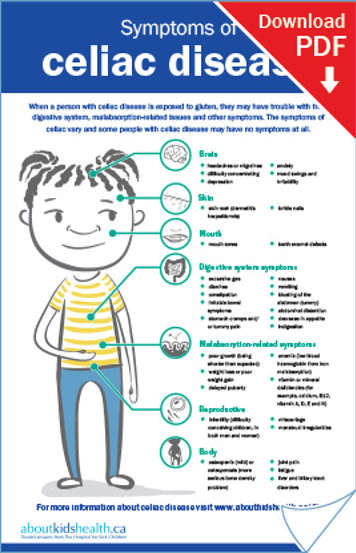
Gastrointestinal system symptoms
When a person with celiac disease is exposed to gluten, they may experience one or more of the following gastrointestinal symptoms:
- tummy pain and/or cramps
- diarrhea
- constipation
- excessive gas
- nausea
- vomiting
- bloating of the abdomen (tummy)
- abdominal distension (expansion)
- decrease in appetite
Malabsorption-related symptoms
They may also experience one or more symptoms that are not related to the gastrointestinal system but are due to nutrient malabsorption. These may include:
- tiredness (fatigue)
- anemia (low blood haemoglobin from iron malabsorption)
- vitamin or mineral deficiencies (e.g. iron, vitamins D and B12.)
- poor growth (not as tall as expected)
- weight loss or poor weight gain
- delayed puberty
Brain
A person with celiac disease may experience one or more symptoms affecting their mental health including:
- headaches or migraines
- difficulty concentrating
- depression
- anxiety
- mood swings and irritability
Skin
People with celiac disease may also experience skin conditions including:
- skin rash (dermatitis herpetiformis)
- brittle nails
Mouth
Symptoms of celiac disease that affect the mouth include:
- mouth sores
- tooth enamel defects
Reproductive
Both males and females with celiac disease may experience issues related to reproduction including:
- infertility (difficulty conceiving children, in both men and women)
- miscarriage
- menstrual irregularities
Body
Other celiac disease symptoms that could affect parts of the body include:
- low bone density, including osteopenia (mild) or osteoporosis (more serious bone density problem)
- joint pain
- tiredness (fatigue)
- liver and biliary tract disorders
Causes, risk factors and prevalence of celiac disease
Celiac disease affects about 1 in 100 Canadians (roughly 350,000 people). It occurs in people all over the world, at any age and from all backgrounds. People develop celiac disease because of a combination of a genetic susceptibility and environmental factors.
People with a relative with celiac disease or who have certain genetic conditions (such as Down syndrome or Turner syndrome) are at higher risk of developing celiac disease.
People who already have one autoimmune condition, such as type 1 diabetes, are at higher risk for developing other autoimmune conditions, such as celiac disease.
How celiac disease is diagnosed
Blood tests
Doctors can order blood tests to screen for celiac disease. These blood tests look for immune proteins (called auto-antibodies) that the body has made in response to gluten in people with celiac disease.
The possible blood tests include:
- Anti-tissue transglutaminase (TTG) antibodies
- Anti-deamidated gliadin peptide (DGP) antibodies
- Anti-endomysial antibodies (EMA)
Your doctor does not need to order all of these blood tests to screen for celiac disease.
Depending on the results, your doctor or health-care provider will talk to you about further testing to confirm celiac disease.
Upper endoscopy
An upper endoscopy may help confirm the diagnosis. An upper endoscopy is a procedure that allows doctors to see the upper part of your child’s gastrointestinal system (from the mouth to the top part of the small intestine). Never start your child on a gluten-free diet before you know for sure whether an upper endoscopy is needed to confirm the diagnosis of celiac disease.

Biopsy of the small intestine
During an upper endoscopy, small pieces of tissue (biopsies) of the small intestine are taken; they will be examined under a microscope. If your child has celiac disease, the biopsy will show that the villi are damaged and flattened in the sample from the small intestine.
Never start your child on a gluten-free diet without first getting a confirmed diagnosis of celiac disease. If a biopsy is done after your child starts a gluten-free diet, your child’s villi may look normal because they will have had a chance to heal since the immune response will have stopped. The biopsy may give a false negative result, which means that the result is negative even though your child has celiac disease.
Talk to your child’s doctor for more information about screening for celiac disease.
Treatment of celiac disease
Celiac disease is a life-long condition. There is no cure or medication for celiac disease. The only treatment is a strict gluten-free diet for life. The diet will help with the symptoms and will keep your child healthy.
Even if your child has no symptoms, once diagnosed your child must follow a strict gluten-free diet for life for treatment of the disease. This means they must remove all sources of gluten from their diet. There are some obvious sources of gluten such as breads, pasta and baked goods. There are also many foods where gluten is hidden, such as soups, salad dressings and ice creams.
Some non-food products may also contain gluten, such as hand creams, medications or arts and crafts supplies like playdough. It is important for your child to limit skin contact with gluten-containing products as it is possible for people with celiac disease to transfer gluten from their skin to their mouth and gut when they are in contact with gluten, which is not safe. Contact with gluten can also trigger skin reactions in some people with celiac disease.
Starting treatment: The gluten-free diet
Once gluten is removed from your child’s diet, the small intestine will start to heal. Your child should start to feel better and symptoms should improve after about six months of being strictly gluten-free.
Maintaining treatment: Sticking to a gluten-free diet for life
Do not stop the gluten-free diet if your child’s symptoms improve. Your child is feeling better because the gluten-free diet is working. If your child stops the gluten-free diet, the villi in the small intestine will become damaged and flattened again, even if they have no symptoms. Any previous symptoms will also return if your child does not follow a strict gluten-free diet.
If your child’s symptoms of celiac disease do not improve after six months, contact your child's doctor.
These tips and resources can help you and your child stick to a strict gluten-free diet.
What happens without a gluten-free diet?
Gluten is toxic to people with celiac disease because it triggers an immune reaction even if your child shows no symptoms.
If your child continues to be exposed to gluten, celiac disease may lead to future health problems including:
- low bone density (osteopenia or osteoporosis)
- some small bowel cancers
- other autoimmune diseases (for example thyroid problems)
- vitamins and mineral deficiencies because of malabsorption
- premature delivery if pregnant
If your child follows a strict gluten-free diet for life, their chances of getting these conditions become the same as the general healthy population.
Children with celiac disease that is not treated are at special risk. Malnutrition during childhood can have significant effects on growth and development. This is why it is so important for your child to remain on a strict gluten-free diet at all times.
Monitoring your child’s symptoms
After the diagnosis, no other upper endoscopy is usually needed. Your child will have more blood tests that check anti-TTG antibody levels. As your child continues a strict gluten-free diet, their antibody levels should lower to normal levels. This may take up to 2 years. High antibody levels tell the doctor that your child was probably exposed to gluten.
Your child’s doctor will also make sure that your child is growing well. If your child had symptoms at the time of diagnosis, they should improve while on a strict gluten-free diet.
When to see a doctor
See your child’s doctor if:
- your child’s symptoms remain after more than six months of following a strict gluten-free diet
- your child’s symptoms worsen
Your child’s doctor may refer you to a dietitian. A dietitian can give you more advice about celiac disease, how to plan a gluten-free diet, and how to get a balance of nutrients while following a gluten-free diet.