What are neuroinflammatory brain disorders?
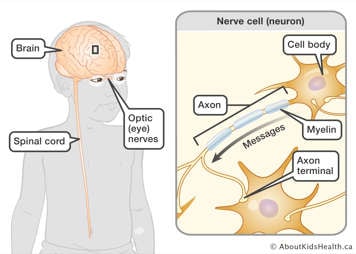
Neuroinflammatory disorders are quite rare but can occur in children. ‘Neuro’ relates to the body’s central nervous system (CNS); ‘inflammatory’ relates to the body’s immune system. The CNS is made up of the brain, spinal cord and optic (eye) nerves.
The immune system is a cellular system that protects our bodies from infections and injury. Sometimes the immune system can over-react and can cause inflammation in healthy tissues in the body. This process is called ‘auto-inflammation’.
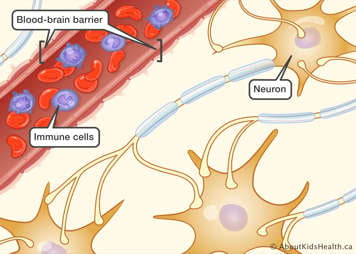
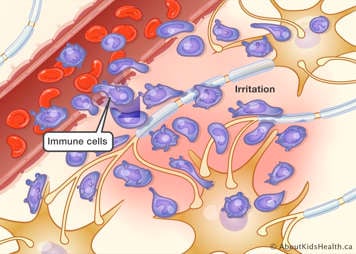
There are many common auto-inflammatory diseases such as eczema, asthma and diabetes. Inflammation of the brain, spinal cord or optic nerves is less common than these conditions, but involves the same process—an over-reaction of the immune system. You can read more about inflammation and the immune system here.
Types of neuroinflammatory disorders
There are many types of neuroinflammatory disorders including antibody-mediated neuroinflammatory disorders, multiple sclerosis (MS), optic neuritis, acute disseminated encephalomyelitis (ADEM), transverse myelitis, autoimmune encephalitis, Rasmussen's syndrome, acute necrotizing encephalopathy of childhood (ANEC), and opsoclonus-myoclonus ataxia syndrome (OMAS).
What are the signs and symptoms of neuroinflammatory diseases?
The signs and symptoms of neuroinflammatory disease can vary depending on which part of the CNS is affected. Inflammation may occur in a distinct location of the CNS, such as the optic (eye) nerves, or multiple locations within the CNS.
Signs and symptoms can include:
- weakness, dizziness or lack of coordination
- loss of normal sensation, seizures
- vision loss
- speech impairment
- memory loss
- decreased alertness
- changes in concentration and behavior
- headache
Other symptoms may include:
- memory or thinking issues
- confusion
- mood swings
What causes neuroinflammatory disorders?
The exact cause of neuroinflammatory disorders is not well understood. Like many auto-inflammatory diseases, it is unknown why the immune system dysfunction occurs. Various theories include exposure to a virus, possible environmental triggers, and genetics.
Diagnosing neuroinflammatory disorder
Several tests will be completed for any child who is experiencing symptoms of suspected neuroinflammatory disorder. Often, magnetic resonance imaging (MRI) of the brain and spine, blood tests, a lumbar puncture and an electroencephalogram (EEG) are completed.
Evaluating signs and symptoms
Your child's medical history and current symptoms will be thoroughly explored. Your child’s health-care team will complete a full physical exam including a complete neurological exam to see what particular signs of inflammation are present, for example movement abnormalities, talking difficulties, etc. They may also do a neurocognitive and psychiatric assessment, for example cognitive dysfunction, memory recall, etc. This will help in understanding what parts of the CNS are affected.
Imaging
Magnetic resonance imaging (MRI) is an imaging procedure that uses radio waves and a large magnet to take pictures of the brain. An MRI provides the health-care team with information that cannot be obtained from an X-ray or computed tomography (CT) scan with the added advantage of zero radiation exposure.
Blood test and lumbar puncture (spinal tap)
Your child’s health team will request a blood sample and a sample of your child's cerebrospinal fluid (CSF)—the fluid that surrounds the brain and spine—to test for viruses, bacteria and other cells. Testing of the CSF is done by conducting a lumbar puncture, also called a spinal tap, and can be helpful to diagnose inflammatory brain disease.
Electroencephalogram (EEG)
An electroencephalogram (EEG) measures the brain's electrical activity. Abnormalities in brain waves are indicative of changes in brain activity. EEGs are used over a period of time to measure improvements in brain activity and to assess how well the brain is working.
Treatment of neuroinflammatory disorders
Treatment goals for neuroinflammatory disease include controlling and reducing inflammation in the CNS with anti-inflammatory medicines and supportive treatments such as anti-seizure medications or physical therapy if needed.
Prednisone
Prednisone is a steroid drug that suppresses (turns off) various immune cells in the body. As a result, prednisone is usually one of the first-line medications used to treat neuroinflammatory disorders. Intravenous (IV) prednisone is given in large doses for 3-5 days to suppress inflammation. Sometimes, oral prednisone may be given for 3-4 months after the IV prednisone, to prevent the inflammation from re-occurring.
Intravenous immunoglobulin
Intravenous immunoglobulin (IVIG) is an intravenously administered blood product that consists of pooled antibodies from hundreds of blood donors. IVIG is a protein that helps to boost your child’s own immune system to reduce CNS inflammation. IVIG is generally well tolerated. Infusion reactions are possible but can be reduced or stopped by medications such as anti-histamines.
Plasmapheresis
Plasmapheresis is a blood filtration procedure, and it involves the removal of blood through a catheter placed in a patient’s vein. The blood is filtered so that the liquid portion called plasma is separated from the cellular portion. The plasma containing inflammatory proteins and antibodies is removed, and the child’s healthy cells are separated and returned along with albumin (a donor blood product like plasma). This procedure is repeated for 5-7 times (cycles) usually every other day. Plasmapheresis works well to ‘wash out’ the inflammatory proteins causing inflammation in the body.
Other treatment options
It is important to note that not all patients will respond the exact same way to these treatments. Various factors impact the disease process as well as the response to treatment. Other treatments may also be added for control of symptoms and side effects such as anti-seizure medications, antibiotics and anti-psychotics.
How to prevent complications
Symptoms and complications of neuroinflammatory disorders can be minimized by following the plan recommended by your child’s health-care team. This can include giving your child immune suppressive medications, performing regular blood testing and imaging, and making sure your child is regularly attending their medical appointments. Providing your child with a healthy balanced diet, adequate sleep and regular physical activity can also be helpful in their recovery.
Complications
Children with neuroinflammatory disorders may experience “flare-ups”, where symptoms of CNS inflammation reoccur. If your child has a flare-up, contact their health-care team so they may be assessed right away. Your child may need to be seen in the Emergency Department and have urgent imaging and testing.
Other complications can include vision loss, balance and co-ordination issues or other neurologic symptoms, which may improve with recovery.
Helping your child
After your child has been diagnosed with a neuroinflammatory disorder they may experience anger, sadness or anxiety. Receiving support or counseling many be helpful. A social worker or counselor can assist your child and family with coping with their diagnosis.
Your child may require additional assistance at home with their activities of daily living or may require additional support at school. Resources and supports can be put in place in the home or school as needed.
What about routine health visits?
Your child’s pediatrician or family doctor will continue to follow your child for routine health visits and if they are ill, for example if your child develops a sore throat.
What about vaccines?
Because many of the treatments for neuroinflammatory disorders suppress the immune system, it is very important that you ensure your child's immunizations are up-to-date. However, while on treatment, your child should not take any live vaccines. Live vaccines are immunizations that use an attenuated form of a virus or bacteria to initiate an immune response. Your child’s health-care team will let you know when it is safe for your child to complete these vaccines. Examples include:
- MMR (measles, mumps, rubella)
- Chickenpox (Varicella)
- Oral influenza vaccine
The health-care team
Your child will be closely monitored by a neurologist who has experience with neuroinflammatory disorders and other members of the neurology team, including nurses and nurse practitioners. Your child may also be followed by other specialty teams such as ophthalmology, rheumatology or immunology.
Clinic visits
It is important to have your child regularly monitored, even if treatment is very successful and your child is feeling healthy. Your child may develop complications that are only mildly symptomatic or absent (asymptomatic) inflammation in the CNS that still require treatment. The health team will also need to monitor the potential effects of treatments by completing regular blood testing and MRI imaging.
At many paediatric hospitals, a child may continue to be followed by a paediatric neurologist until they are 18 years of age. When they turn 18, they will need adult care. Your child's neurologist will be able to tell you what to expect in terms of visits and how to transition to adult neurology care.
When to seek medical attention
Contact your child's neurology team, call 911 or go to the nearest Emergency Department right away if your child experiences any of the following:
- A seizure
- Changes in their level of consciousness
- Difficulty seeing
- Problems speaking or swallowing
- Balance issues