What is congestive heart failure?
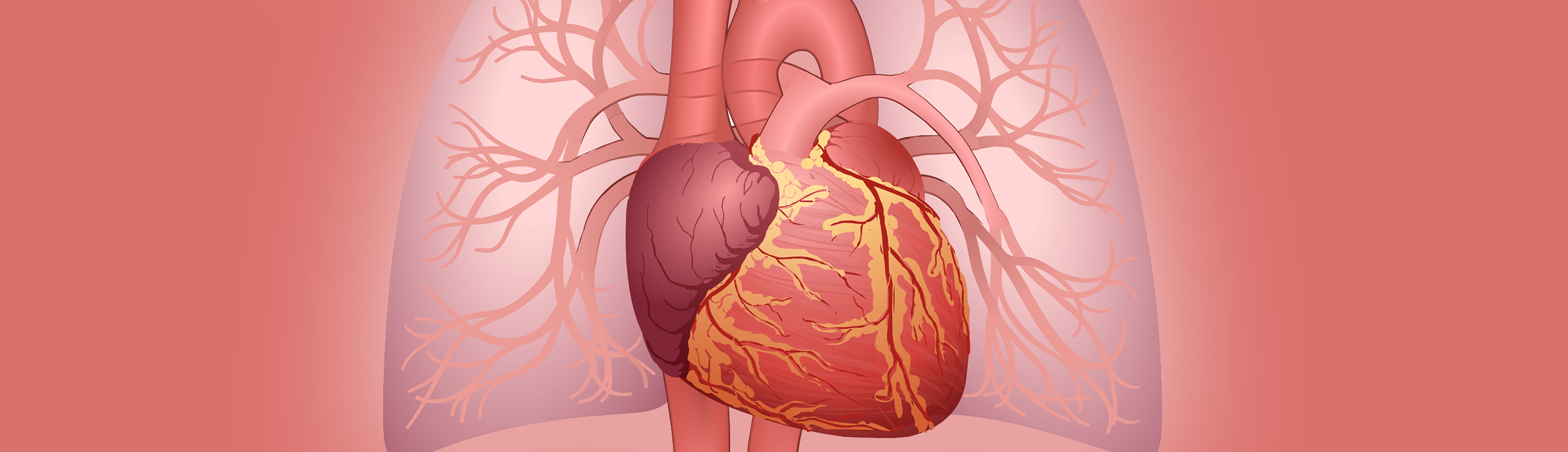
Congestive heart failure (CHF) is a condition in which the heart does not pump as well as it should. When there is not enough blood pumped from the heart, this is described as low cardiac output. CHF can lead to different problems, depending on which side of the heart is affected.
There are two sides of the heart: the right side and the left side. The right side of the heart pumps blood to the lungs, where the blood picks up oxygen. The left side pumps blood to the rest of the body. CHF may affect only one side of the heart, while the other side still pumps blood normally.
Common problems caused by CHF include:
- The right side of the heart receives blood from the body's veins. If this side is not pumping as well as it should, blood returning to the heart backs up in the veins. When this happens, fluid collects in the body tissues. In babies and children, you may see this fluid as swelling (edema) or puffiness around your child's eyes, hands, feet, and belly.
- The left side of the heart receives blood from the lungs. When the left side is not pumping well, fluid backs up into the lungs. If this happens, you may notice that your child's breathing becomes noisy, difficult, and faster.
- Both sides of the heart can be connected with a hole that allows blood to pass through in an abnormal way. Like problems with the left side of the heart, this can lead to extra fluid in the lungs. This may cause breathing problems. It may also make it harder for your child to feed and gain weight.
What are the symptoms of heart failure in children?
The way children show signs and symptoms of heart failure can vary depending on their age and can change over time. Infants with heart failure often have poor weight gain, struggle to meet developmental milestones, feed poorly, and sweat excessively with crying or feeding. Older children may become tired or fatigued easily when playing, have abnormal heart rhythms, and/or difficulty gaining weight or keeping weight on.
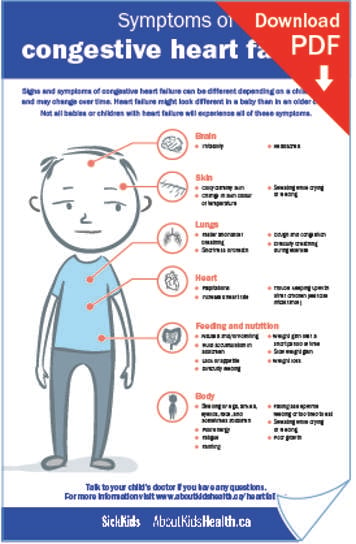
Symptoms of heart failure can affect different areas of the body:
Brain
- Irritability
- Headaches
Skin
- Cold, clammy skin
- Change in skin colour or temperature
- Sweating with crying or feeding
Lungs
- Faster and harder breathing
- Shortness of breath
- Coughing and congestion
- Difficulty breathing during exercise
Heart
- Palpitation
- Increased heart rate
- Trouble keeping up with other children physically (i.e. while running or playing)
Feeding and nutrition
- Nausea or vomiting
- Fluid buildup in the abdomen (belly)
- Poor appetite
- Difficulty feeding
- Gain a lot of weight over a short period of time
- Slow weight gain
- Weight loss
Other symptoms
- Poor energy
- Fatigue (feeling extremely tired or weak)
- Fainting
- Falling asleep while feeding or too tired to eat
- Poor growth
- Swelling of face, eyelids, legs ankles and sometimes abdomen (rare).
Not all infants or children with heart failure will experience all of these symptoms.
What causes congestive heart failure in children?
Children of all ages can develop congestive heart failure. However, the causes of heart failure in children are typically very different from the causes of heart failure in adults.
Some children are born with malformations to their heart, also known as congenital heart disease (CHD). Some types of CHD may require one or more surgeries, often starting in infancy. In some cases, a child may develop symptoms of heart failure despite having surgery.
Some children may not have structural problems with their heart, but there is a problem with the way the heart either squeezes (contracts) or relaxes. There are also metabolic conditions, which affect the way the body uses energy, and genetic disorders that are linked with heart failure in children. Changes in certain genes, which are the building blocks to our bodies, have been found to be responsible for both CHD and cardiomyopathies, diseases of the heart muscle that cause it to become enlarged, thick, or stiff. Ongoing research is being done to better understand the role genes play in heart conditions and heart failure.
Children can also develop heart problems later in life that may result in heart failure. This can be caused by infections or inflammation of the heart, which cause the heart muscle to function poorly. This condition is called “myocarditis.”
Some medications used to treat other conditions or diseases can be toxic to the heart. Certain chemotherapy medicines, used to fight cancer, can also lead to changes in heart function over time.
How is heart failure diagnosed in children?
If your child’s doctor suspects your child has heart failure or is at risk of developing heart failure, your child may be referred to a paediatric heart specialist. This is a doctor who is trained in assessing heart function in children.
Your child will likely have a series of diagnostic tests including an electrocardiogram (ECG), a chest X-ray or an echocardiogram (heart ultrasound). Blood work may also be done to examine how other organs are working or to find a genetic explanation for your child’s heart failure. If your child has a family history of heart conditions or cardiomyopathy, your doctor may recommend that you meet with a genetic counsellor who specializes in cardiac diseases.
Diagnostic lab tests
Electrocardiogram (ECG)
- For an ECG, a technician will put stickers on your child’s chest.
- Your child will need to lie still for one to two minutes while the technician records the rhythm of your child’s heart.
- Do not worry; your child’s health-care team will help keep your child calm during the test.
Echocardiogram
- An echocardiogram is an ultrasound of the heart that allows the doctor to see the structure of the heart and how the heart squeezes or relaxes. This test does not have any radiation.
- This test takes between 45 minutes to one hour. Your child will need to lie still for this time.
- If your child is aged between three weeks and three years or if they are unable to lie still, they will need a sedative or general anaesthesia to help them relax or fall asleep for the test. Your child will not be allowed to eat or drink anything for several hours before taking the sedative and having the general anaesthetic.
- If your child is too old for sedation, the health-care team will use other techniques to keep them distracted and as still as possible during the test.
Chest X-ray
- A chest X-ray is a picture that gives information on the size of the heart and the presence of any fluid in the lungs.
- Since taking a chest X-ray requires a certain position, young children need to be placed in a holder that allows them to be upright with their arms up. This might be frightening for some parents, but it is a very quick test and it is necessary to obtain good pictures.
Blood test
- Blood tests are often done to look at the function of other organs and measure hormones that can be elevated in heart failure.
- These tests often need to be repeated once any heart medications are started as a way to monitor how a child is doing.
Genetic testing
- If you or your child are diagnosed with certain conditions or if you have a strong family history of cardiomyopathy, your cardiologist may recommend your family meet with a genetic counsellor.
- The genetic counsellor will take a detailed family history.
- The genetic counsellor will explain to you and your family what the role for genetic testing is for your child, the chances that testing will be informative and explain the implications of a positive or negative genetic test. They will also discuss the risks of another child or another member of the family having a similar condition.
- The Heart Centre Biobank is a research initiative through which newer tests for heart failure are being developed. You may be approached to participate in the biobank for future research (www.heartcentrebiobank.ca). Your child’s level of care will not be affected by your decision to participate or not.
Cardiac magnetic resonance imaging (or cardiac MRI)
- A cardiac MRI gives detailed information on how the heart is built and functions. An MRI does not use X-ray radiation. Not all children will need a cardiac MRI.
- For this test, your child will lie down inside a large, round machine with a wide tunnel at the centre. The scanner makes a loud knocking or drumming sound during the scan. The technologist can communicate with your child through a speaker. Some scanners have an entertainment system so your child will be able to watch a movie while having the scan.
- A cardiac MRI scan usually takes between 45 minutes to one hour to complete. Additional time may be needed to prepare for the MRI. Since young children are unable to lie still for this long, they may receive a sedative or general anaesthetic to make them sleep during the scan.
Cardio-pulmonary exercise stress test
- Usually starting at the age of eight years, children may be asked to perform exercise testing.
- There are two types of exercise tests:
- The first type is to find out how the heart and lungs interact and how energy is used during exercise. This is done on a stationary bicycle and requires your child to breathe into a mouth piece similar to what is used in scuba diving.
- The second test looks at heart rhythm during exercise. This one is performed on a treadmill and does not include any breathing equipment.
- Your child’s condition and coordination will determine the type of exercise test that is required.
Cardiac catheterization
- Cardiac catheterization can be done for several reasons:
- To obtain more information on the pressures inside your child’s heart
- Evaluate the arteries and vessels of the heart for narrowing or blockages
- To obtain a tiny piece of heart muscle (also called a biopsy) for specialized testing
- In some cases, catheterization may be done as a treatment for heart failure.
- This test requires general anesthesia. Your child will not be allowed to eat or drink anything for several hours prior to the test.
Treatment of heart failure in children
The treatment of heart failure in children often depends on the cause of the underlying problem. Sometimes there are medical, surgical or catheter-based interventions that can be undertaken to either cure or reduce the symptoms of heart failure. Your child will be taken care of with a team that includes physicians, nurses, specialized dieticians who ensure optimal nutrition, and physical and occupational therapists who will provide assessments. Your child will be prescribed medicines to treat both the symptoms of heart failure and to improve or stabilize heart function. Child life specialists and social workers are available to help children and families dealing with the stress associated with a chronic illness.
Depending on your child’s condition, they may also benefit from supportive therapies such as feeding support and CPAP (continuous positive airway pressure).
Medications
Your child may be given different medications to help treat CHF. Medications that are commonly prescribed to treat CHF in children include:
- Inotropes: Given by IV, these medications encourage the heart to beat more strongly.
- Angiotensin-converting enzyme (ACE) inhibitors: These medications are used to stabilize or improve the amount of work the heart has to do to pump blood.
- Beta blockers: Work by decreasing blood pressure and slowing the heart down. This allows the heart to beat more slowly and steadily.
- Diuretics: Help remove extra fluid that can build up in the body as a result of heart failure.
- Anticoagulants: Also known as blood thinners, these drugs stop clots from forming in the blood.
Implantable cardioverter defibrillator (ICD)
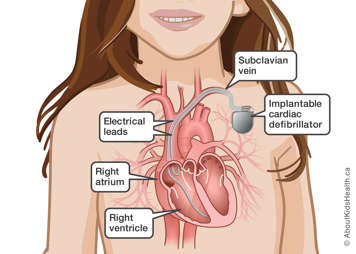
Some types of heart disease can increase the risk of a sudden cardiac arrest due to an abnormal heart rhythm. If your child has suffered a sudden cardiac arrest or they are considered high risk to have a sudden cardiac arrest, and if your child is old enough, they may be given an implantable cardioverter defibrillator (ICD). An ICD is a specialized pacemaker. It is able to help the heart beat faster if it beats too slowly, and detect and treat fast rhythms by either slowing down the heart or delivering a shock to the heart (defibrillation) to put it back into a normal rhythm.
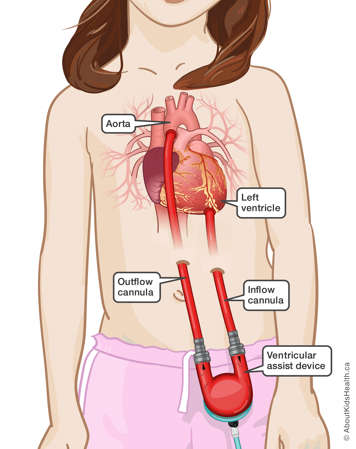
Ventricular assist devices (VAD)
Sometimes, despite medical therapy, heart failure can progress to a very advanced stage where the heart is unable to pump blood to other organs in the body. In these situations, your child may need an artificial heart pump or heart-lung machine to support their heart function. In some cases, this may be temporary to give the heart a rest and help it to recover. In other cases where heart failure has reached end-stage, where there is little chance for recovery, these machines may be used to support your child while waiting for a heart transplant. The most common form of this type of support is a ventricular assist device also called a “mechanical heart.” However, due to the current limitations of technology not all device therapies are suitable for all children.
Heart transplantation
Another form of life-saving therapy is a heart transplant. Although the failing heart is replaced, receiving a new heart will require your child to be on lifelong immunosuppressant medications to stop your child’s body from rejecting the new heart. Although necessary, these medications can increase the risk of infection, kidney problems and cancer. Strict criteria must be met to be a candidate for a heart transplant. Depending on their condition, not every child is a candidate to receive a heart transplant. The process of evaluation for transplant, listing for transplant, and management after transplant is complex. To determine if your child is a suitable candidate for a heart transplant, they will need to undergo a series of tests and meet with all members of the transplant team.