What is an infantile hemangioma?
Infantile hemangiomas are the most common, non-cancerous growths in babies. They are caused by extra growth of cells lining the small blood vessels in the skin. These cells are called endothelial cells.
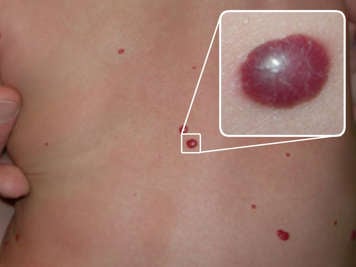
Some infantile hemangiomas sit on top of the skin and have red-purple skin changes, which are flat or raised. Deep hemangiomas under the skin appear as a skin-coloured bump that may have a blue hue. Some hemangiomas have both components. They are soft to touch and do not cause pain unless the skin above is broken or ulcerated. About 60 per cent of hemangiomas occur on the head and neck, but they can occur anywhere on the body. Rarely, they can occur inside the body as well.
Infantile hemangiomas normally appear in the first two weeks of life. Deeper hemangiomas may not appear until two to three months of age. About 30 to 40 per cent of hemangiomas appear at birth as a barely visible spot, either slightly dusky or coloured differently than the skin around them.
Who is at risk of having an infantile hemangioma?
Infantile hemangiomas are more common in individuals who are born female, twins, premature babies and babies who are born with a low birth weight.
We do not know what causes hemangiomas or how to prevent them.
Infantile hemangiomas usually get smaller as your child gets older
Infantile hemangiomas occur in as many as 5 per cent of babies. They grow the fastest during the first five to seven weeks and reach the ultimate size by several months of age. Most of them stop growing by five to six months of age.
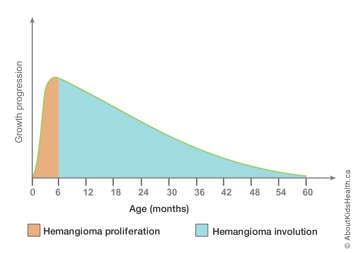
Infantile hemangiomas often follow a predictable pattern of growth (proliferation) and getting smaller (involution). This means they usually get smaller as the child gets older.
| Age (approximate) | Hemangioma phase |
|---|---|
| 0 to 4 months | Proliferation (growth) is rapid |
| 4 to 6 months |
Plateau; growth is very slow or stopping |
| 12 to 60 months (5 years) |
Involution (getting smaller) |
The size, the location and the way the infantile hemangioma looks will not affect how fast it grows or shrinks. After the hemangioma stops growing, your child may still have loose skin, a change in skin colour or a change in the way the skin feels (texture). Sometimes, there will be small blood vessels (telangiectasia) that stay on the skin.
Testing for hemangiomas
Usually, your child's health-care provider can diagnose an infantile hemangioma by looking at it. Tests are not needed in most cases. Depending on the location of the hemangioma, your child's health-care provider may run tests (such as ultrasound or MRI) to see if the hemangioma affects other parts of your child's body. They may ask for a consultation from other specialists to make sure the hemangioma does not affect breathing and vision and to assess the depth of the hemangioma.
Treatment for hemangiomas
Most infantile hemangiomas require no treatment or testing as most go away on their own and are not associated with other problems. Your child's health-care provider may suggest a "wait and see" approach. This means waiting to see what happens on its own before treating the hemangioma.
If your child's hemangioma is on the skin and requires treatment, they may be referred to a dermatologist. A dermatologist will decide if the hemangioma needs to be treated by considering:
- location of the hemangioma on the body
- size, shape and rate of growth of the hemangioma
- age of your child
- risk and benefits of treatment
Medicine, surgery and laser treatments are options at different stages of hemangiomas, if needed. They can be discussed with your child's primary care provider or dermatologist.
Treatment options for hemangiomas that are growing may include the following medicines:
- topical gel known as timolol (an eye drop that can help to shrink small hemangiomas)
- beta-blockers (propranolol, nadolol) taken by mouth
- laser treatment may be helpful to stop bleeding hemangiomas. It may also help to improve redness or fine blood vessels if they persist after the hemangioma has gone away or involuted
Hemangiomas that are found deeper in the body may be evaluated by other specialists, depending on the location of the hemangioma.
Complications of infantile hemangiomas
If your child has an infantile hemangioma on or near the eyes, nose, ears, lips or neck, it might affect their ability to see or breathe.
Infantile hemangiomas may develop a wound (ulcer), which can cause bleeding or become infected and cause pain, especially if the hemangiomas are near diaper areas, skin folds and the lips.
Infantile hemangiomas may leave a change in skin colour or a change in the skin texture, which can be a cosmetic concern for some people.
Treating bleeding
If your child's hemangioma starts to bleed, follow these steps:
- Apply pressure to the site for 15 minutes.
- If the bleeding does not stop after 15 minutes, take your child to the closest Emergency Department.
Coping with an infantile hemangioma
If your child with a hemangioma is a baby or toddler, talk to your daycare staff and to parents of other children that attend the day care about hemangiomas. Explain that your child has this condition and that it will not spread to other children.
School can cause a great deal of stress in children with infantile hemangiomas. By the time children attend grade school, they are old enough to realize that they look different than other children. Parents, family members and teachers should understand the stress these children experience and that these children may need more emotional support and understanding.
Talk to your child about diversity, bullying and acceptance
Talk to your children about hemangiomas and address topics such as diversity, bullying at school and acceptance. Children with hemangiomas often have to endure hurtful comments from other children, even when they are young. They may feel uncomfortable in social situations or self-conscious about their skin. Remind your child that they are not to blame for their hemangioma.
