The kidneys are important organs in our bodies. They help to keep us healthy in many ways.
- They take waste products, such as urea and creatinine, away from the body.
- They control the water balance in the body.
- They control the balance of other substances in the body, such as sodium and potassium.
- They help make red blood cells.
- They help bones grow.
- They help control blood pressure.
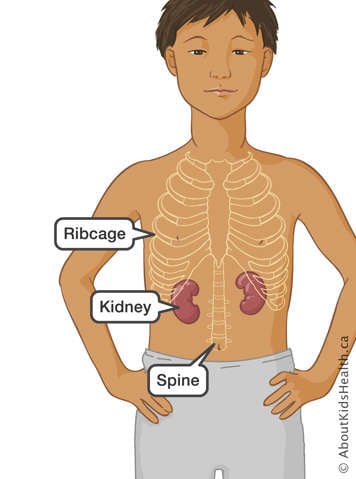
Most people have two kidneys, one on each side of the spine, just under the rib cage. They are red-brown in colour and about the size of your child's fist.
What happens in chronic kidney disease?
When your child has chronic kidney disease (CKD), their kidneys have had changes in how they were formed or how they function and have stopped working normally for at least three months or longer. This can lead to a build-up of unwanted substances in the blood.
CKD is categorized by its severity—the cause of the kidney issues, how well the kidneys filter waste (estimated glomerular filtration rate [eGFR]), and the amount of protein in the urine. If the kidneys develop a severely reduced ability to function, it is called kidney failure.
Kidney disease stage and function
| Stage | Description | Kidney function/eGFR |
|---|---|---|
| 1 | Possible kidney damage (e.g., protein in the urine) with normal kidney function | 90-100% |
| 2 | Kidney damage with mild loss of kidney function | 60-89% |
| 3a | Mild to moderate loss of kidney function | 45-59% |
| 3b | Moderate to severe loss of kidney function | 30-44% |
| 4 | Severe loss of kidney function | 15-29% |
| 5 | Kidney failure | Less than 15% |
CKD is progressive, meaning it can get worse over time and may require treatment. How fast it progresses depends on many factors including illness, dehydration, growth spurts, protein in the urine, and high blood pressure.
Build-up of creatinine
Creatinine is a waste product. High levels of creatinine mean the kidneys are not filtering well. Creatinine levels can be affected by hydration, infection, or blockages. Kidney function is measured by filtration rate (eGFR). Normal eGFR is about 100. If eGFR is 30, the kidneys are working at 30% of normal.
Build-up of urea
The body produces urea when it breaks down or uses proteins. Urea is a waste product, so healthy kidneys remove it through urine (pee). When the kidneys are not healthy, however, the urea builds up in the blood, leading to a condition known as uremia.
If your child has uremia, they might:
- urinate (pee) very little or not urinate at all
- have a low appetite
- feel nauseous
- feel tired
- feel cranky
- feel itchy
- have trouble concentrating.
Build-up of other minerals
Usually, healthy kidneys remove excess potassium and phosphate from the body. When kidneys start to fail, these wastes build up in the blood. Sodium and calcium can be high or low in the blood based on the stage of kidney disease and underlying kidney issues.
Puffiness in the feet, hands and eyes
This type of puffiness is called edema. It occurs when fluid builds up in the body because the kidneys make less urine.
Pale skin and fatigue
Red blood cells contain hemoglobin, which carries oxygen to all parts of the body. Kidneys help make red blood cells; but, when the kidneys do not work very well, they do not make the cells quickly enough (anemia). This causes your child to become pale and have less energy.
Headache and irritability
Your child might become irritable if they have a build-up of urea or if they have hypertension (high blood pressure). Blood pressure rises either because of the extra fluid in your child's body or because of a hormone called renin. The kidneys make renin when they are scarred or do not get enough oxygen from the blood.
Poor growth
Kidneys keep the blood's acid-base balanced. When kidneys do not function properly, the blood becomes too acidic, causing poor growth and weak bones. Children with CKD may also have poor appetites and deficiencies of some vitamins. Monitoring of growth and nutrition is an important part of the care of children with CKD.
Treatments for chronic kidney disease
Treatment for CKD depends on its severity and can include:
- medications to control blood pressure
- optimizing growth and nutrition
- preventing further injury to the kidneys by avoiding certain medications.
Fluid intake
How much fluid your child should drink is based on their urine output. It is important to measure and keep track of fluid intake. You will be asked to collect your child’s urine over a 24-hour period to make sure your child is drinking enough.
Medications
It is important to avoid medicines that can harm the kidneys like nonsteroidal anti-inflammatory drugs (NSAIDs) used for pain relief and fever reduction (e.g., ibuprofen, naproxen). Tell your child’s health-care providers about your child's CKD for safe prescriptions.
High blood pressure (hypertension)
When your child’s kidneys are damaged, their blood pressure can go up. A low-salt diet and medicines can be used to control high blood pressure. A 24-hour blood pressure monitor and heart ultrasounds may be used to check your child’s heart health.
Anemia
When the kidneys do not work very well, the body stops making enough red blood cells (anemia). Anemia is treated with iron supplements and medicines given by injection every one to four weeks.
Bladder and bowel function
Depending on the kidney condition, your child may need help from a urologist to keep the bladder and bowels working well. This may include treating constipation and urinary tract infections.
Bone health
Low kidney function can cause weak bones and calcium build-up in the heart and blood vessels. Your child may need calcium supplements, phosphate binders, and different forms of vitamin D to help.
Growth
CKD can affect growth in children. Growth hormones may be used to help your child grow until they receive a transplant (if required) or reach their expected height. If your child can't eat enough, a feeding tube may be suggested to take in enough nutrients. A dietitian can also help create a diet plan for your child.
Activity
Your child should engage in at least 60 minutes of physical activity each day. Exercise helps strengthen bones, control blood pressure, keep a healthy body, and improve mental health.
Treatments for kidney failure
Depending on the underlying cause of CKD, the progression of CKD can be slowed in some children. In others, CKD can worsen over time. Kidney failure, the most severe stage of CKD, requires kidney replacement therapy.
Kidney replacement therapy includes:
- kidney transplant
- dialysis.
Kidney transplant
- This involves surgery (an operation) to place a healthy kidney from a donor into your child's body.
- A kidney can come from a living donor or a deceased donor who is a match for your child. If a child is waiting for a kidney from a deceased donor, they go on a transplant waiting list.
- When your child receives a new kidney, they will need to take medications every day to suppress, or weaken, their immune system so that they do not reject it.
Dialysis
Patients and families can choose between two types of dialysis:
- hemodialysis
- peritoneal dialysis.
It is important to learn the facts about each type of dialysis before choosing one. You will also need to consider if you want to do the dialysis at the hospital or in the comfort of your own home. Keep in mind that your child may need to change from one kind of dialysis to another, depending on their health.
Hemodialysis
There are two types of hemodialysis: home hemodialysis (HHD) and in-hospital hemodialysis.
Home hemodialysis:
- uses a vascular access (a thin tube inserted in a vein) or an AV fistula to clean your child's blood
- is a slow, gentle treatment that improves your child's appetite and energy levels
- occurs every day over the course of eight to 10 hours (usually overnight)
- requires your child to take fewer medications (compared with in-hospital dialysis)
- allows your child to have a wider range of foods and drinks.
Home hemodialysis may only be offered to patients who are expected to wait a longer period of time for a transplant.
In-hospital hemodialysis:
- uses a central venous catheter (CVL) or an AV fistula to clean your child’s blood
- is offered and monitored by qualified health-care professionals
- is done in a clean, friendly and supportive environment over the course of 3 to 4 hours
- occurs three to four times per week
- gives your child the chance to meet other patients.
Peritoneal dialysis
- Peritoneal dialysis (PD) uses a thin tube called a catheter and the inner membrane (lining) of the abdomen to clean the blood.
- PD offers flexible, easy treatments at home, where you or your child can manage the care.
- PD may help preserve urine output and remaining kidney function.
Choosing the treatment option that suits best
It is important to learn about kidney disease and how to manage it. This will help decide what treatment matches your child’s lifestyle.
For extra guidance, try out this decision-making tool from Ottawa Hospital Research Institute. It is designed to guide people through any health-related or social decision and may help you choose which treatment is best for you and your child.
Being active members of the kidney care team
Remember, you and your child are the most important members of your child's nephrology (kidney care) team. The nephrology team will support and guide you to gain confidence to manage your child's kidney disease.
Your commitment to the treatment and your positive attitude will result in better outcomes for your child's health. Staying active and encouraging a healthy lifestyle are also essential for the long-term success of your child's treatment.
Coping with chronic illness
When your child is diagnosed with CKD, it is normal to feel upset and angry. It is okay to feel sad as you adjust to these feelings and changes in your family’s life. Everyone reacts differently to a new diagnosis. Look to your child’s health-care team to help with your coping and mental health.
For more information on how to cope with chronic illness, see Living with a chronic condition: Overview and Coping with your child's illness as a parent.
At SickKids
The Chronic Kidney Disease (CKD) clinic consists of a group of multidisciplinary professionals who will help you and your child look after your child’s kidney health including pediatric nephrologists, nurse practitioners, registered nurses, renal dieticians and social workers. A dietitian can help with your child’s food needs, growth, vitamins, and healthy living tips. A social worker can help with adjusting to the diagnosis of kidney disease, following treatment, finding resources, providing emotional support and stress management, and transitioning to adult care.
The clinic helps with kidney health for children with CKD stages 3b to 5, and sometimes earlier stages if needed. We aim to keep the kidneys working as well as they can, manage your child’s symptoms, and help with living with CKD. We will look at your child's medical history and perform physical exams, lab tests, and genetic tests to find out the cause of your child’s CKD.
This care does not replace your child's regular health-care provider who takes care of things like check-ups, vaccines, and other illnesses.
Clinic visits
The clinic sees patients every one to four months, depending on their CKD level. Babies may need to come once or twice a week. Clinics are on Monday mornings from 8 am to 12 pm. Visits can last up to three hours, so bring snacks, water, and something to do for your child. The clinic also offers virtual appointments on Mondays or Thursdays. Older children may be asked to get blood tests one to two weeks before their visit.
Who to contact
You can reach the clinic’s two nurse practitioners (NPs) by phone or email during weekdays from 8 am to 5 pm. They will talk to you about medicine changes, health updates, test results and care plans. Please allow up to 72 hours for a reply.
Urgent Issues
For urgent problems, go to your local Emergency Department or call the on-call nephrologist at 416-813-7500. Urgent problems include fever, less urine due to dehydration, signs of a urinary tract infection, or changes in your child’s behaviour. Prescription refills are not urgent and can be handled the next day.
Finding out more about treatment options
You can find out more about the different treatment options on the following pages.
- Hemodialysis
- Home hemodialysis
- In-hospital hemodialysis
- Peritoneal dialysis
- Dialysis options: How they compare
Resources
About Kids Health
- Nephrology learning hub – https://www.aboutkidshealth.ca/learninghub/nephrology2/?language=en
- Mental health learning hub – https://www.aboutkidshealth.ca/learninghub/mental-health/?language=en
National Kidney Foundation – https://www.kidney.org
- Children with CKD: Tips for Parents – https://www.kidney.org/kidney-topics/children-chronic-kidney-disease-tips-parents
Kidney Foundation of Canada – www.kidney.ca (EN) https://rein.ca/ (FR)
National Institute of Diabetes and Digestive and Kidney Diseases (NIH) – https://www.niddk.nih.gov/
- Helping Your Child Adapt to Life with Chronic Kidney Disease – https://www.niddk.nih.gov/health-information/kidney-disease/children/helping-child-adapt-life-chronic-kidney-disease?dkrd=/health-information/kidney-disease/children/caring-child-kidney-disease#eating
My Kidneys My Health – https://mykidneysmyhealth.com/
My Renal Nutrition: Living with Kidney Disease – https://www.myrenalnutrition.com/living-kidney-disease
Your Child’s Mental Health – https://caringforkids.cps.ca/handouts/mentalhealth/mental_health
Department of Pediatrics and Child Health: Healthy Kidneys – https://mbpedchildhealth.ca/healthy-kidneys-resources/
References
Stevens, Paul E. et al. KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney International, Volume 105, Issue 4, S117 – S314.
Isakova, Tamara et al. KDOQI US Commentary on the 2017 KDIGO Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease–Mineral and Bone Disorder (CKD-MBD). American Journal of Kidney Diseases, Volume 70, Issue 6, 737 – 751.